Introduction
Jaundice refers to the yellow discoloration of skin and sclera caused by elevated bilirubin levels in the blood. Understanding its types—pre-hepatic, hepatic, and post-hepatic—is crucial for diagnosis and treatment.
What is Jaundice?
- Definition of jaundice (bilirubin > 35–40 μmol/L)
- Pathophysiology: excess bilirubin from hemolysis, liver dysfunction, or biliary obstruction
- Key visual clue: yellow sclera and skin
Types of Jaundice
1. Pre-Hepatic (Haemolytic) Jaundice
Increased unconjugated bilirubinCommon causes:
- Hereditary spherocytosis
- Thalassemia
- Sickle cell disease
- G6PD deficiency
2. Hepatic (Hepatocellular) Jaundice
Damage to hepatocytes; mix of conjugated and unconjugated bilirubinCommon causes:
- Viral hepatitis (A, B, C, EBV)
- Alcoholic hepatitis
- Drug-induced (paracetamol, halothane)
- Gilbert’s and Crigler-Najjar syndromes
3. Post-Hepatic (Obstructive) Jaundice
Obstruction of bile flow, ↑ conjugated bilirubinCommon causes:
- Gallstones
- Cholangiocarcinoma
- Pancreatic head tumor
- Portal lymphadenopathy
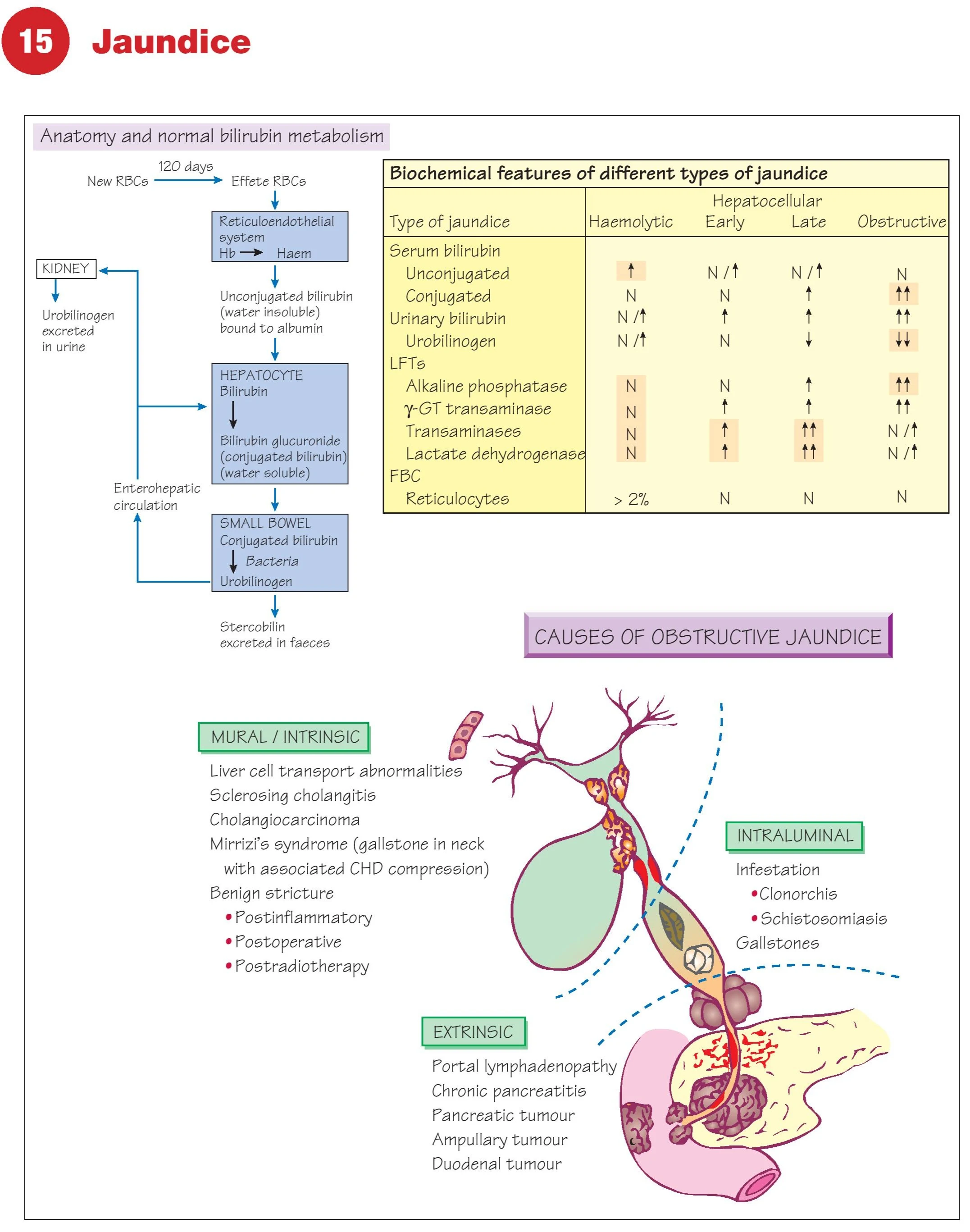
Bilirubin Metabolism Simplified
- Breakdown of old RBCs → heme → unconjugated bilirubin
- Conjugation in liver → excretion into bile → stercobilin in feces, urobilinogen in urine
- Diagram reference: from hemoglobin to urine and stool pathways
- Importance of distinguishing water-soluble (conjugated) vs insoluble (unconjugated)
Biochemical Differences in Jaundice Types
| Feature | Hemolytic | Hepatocellular (Early) | Hepatocellular (Late) | Obstructive |
|---|---|---|---|---|
| Serum bilirubin | ↑ unconjugated | ↑ mixed | ↑ conjugated | ↑ conjugated |
| Urinary bilirubin | Normal | ↑ | ↑↑ | ↑↑↑ |
| Urobilinogen | ↑ | ↓ or ↑ | ↓↓ | ↓↓↓ |
| ALP, γ-GT | Normal | Mild ↑ | Mild ↑ | Marked ↑↑ |
| Transaminases | Normal | ↑↑ | ↑ or N | Normal |
| Reticulocytes | >2% | Normal | Normal | Normal |
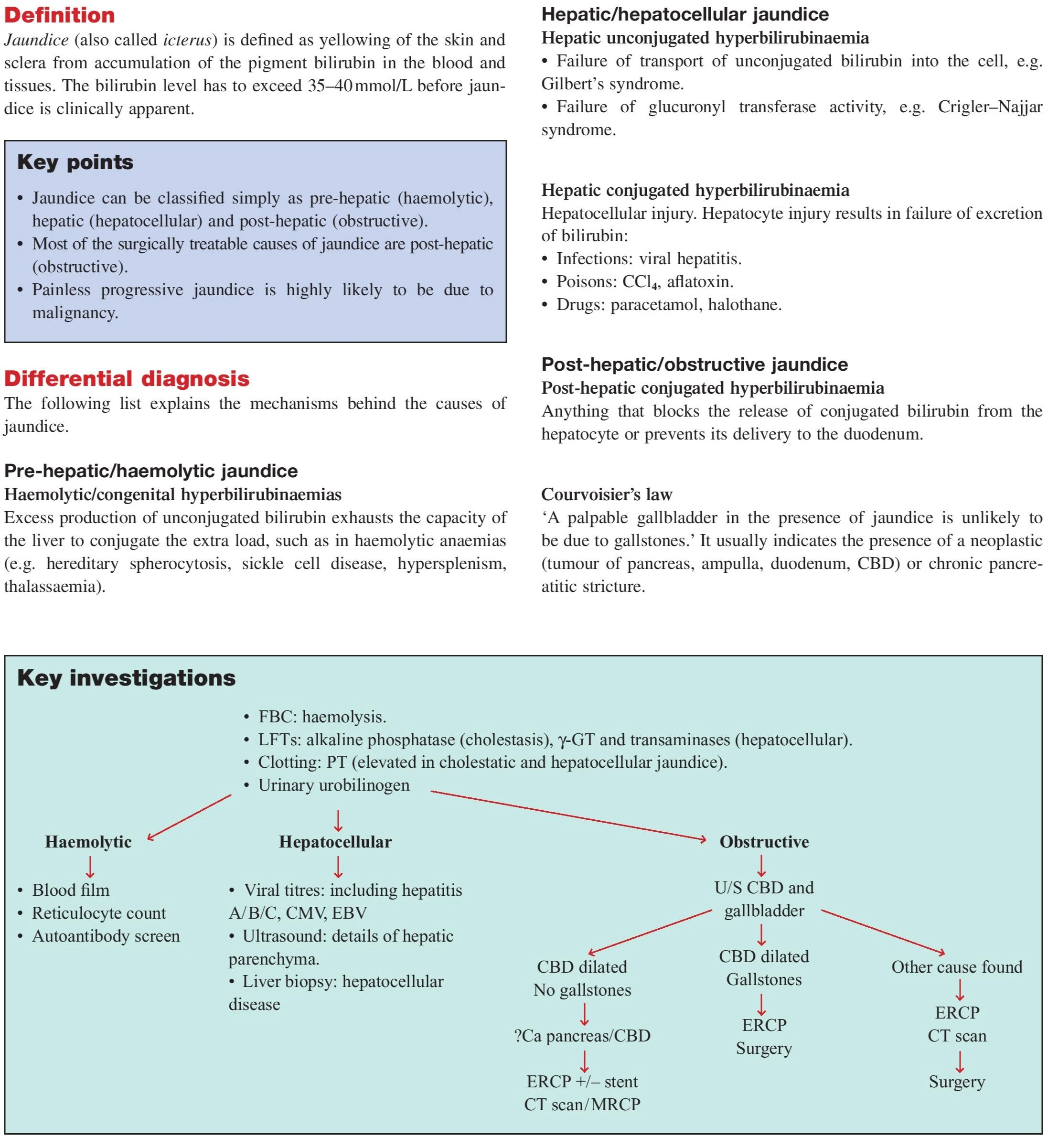
Causes of Obstructive Jaundice
Mural (Intrinsic to bile duct wall)
- Sclerosing cholangitis
- Cholangiocarcinoma
- Mirizzi’s syndrome
- Post-inflammatory or post-radiotherapy stricture
Intraluminal
- Gallstones
- Clonorchis, Schistosoma infection
- Parasites blocking ducts
Extrinsic Compression
- Pancreatic carcinoma
- Portal lymphadenopathy
- Ampullary or duodenal tumor
- Chronic pancreatitis
Courvoisier’s Law
A palpable gallbladder in the presence of jaundice is unlikely due to gallstones—often pancreatic head tumor.
Clinical Features of Jaundice
Color changes: yellow sclera → skin
Dark urine, pale stools: suggest obstructive typeItching: due to bile salt accumulation in skin
Associated symptoms:
- Fever, RUQ pain (cholangitis)
- Weight loss, anorexia (cancer)
- Hepatomegaly or gallbladder enlargement
Differential Diagnosis
| Type | Common Causes |
|---|---|
| Pre-Hepatic | Hemolysis (sickle cell, G6PD, thalassemia) |
| Hepatocellular | Hepatitis, paracetamol toxicity, alcohol, EBV |
| Obstructive | Gallstones, pancreatic cancer, CBD strictures, cholangiocarcinoma |
Key Investigations
| Test | Purpose |
|---|---|
| FBC | Anemia, leukocytosis, reticulocytes (hemolysis) |
| LFTs | Distinguish obstructive (↑ALP) vs hepatocellular (↑AST/ALT) |
| Clotting (PT) | Prolonged in cholestasis and liver failure |
| Urinary urobilinogen | Increased in hemolysis, decreased in obstruction |
| Viral serology | Hepatitis A/B/C, CMV, EBV |
| Ultrasound | Bile duct dilatation, gallstones, gallbladder mass |
| CT scan | Pancreatic tumors, liver lesions |
| ERCP | Diagnostic and therapeutic for obstructive jaundice |
| MRCP | Non-invasive imaging of biliary tree |
| Liver biopsy | Confirm hepatitis, cholestasis, malignancy |
Diagnostic Flow
Suspect Hemolysis
→ Blood film, Reticulocyte count, Autoantibody screen
Suspect Hepatitis
→ Viral serology, USG liver, ± biopsy
Suspect Obstruction
→ USG CBD → CT/ERCP → Surgery if tumor or strictures confirmed
FAQs
Is jaundice always a liver problem?
No. It can be pre-hepatic (hemolysis), hepatic (liver), or post-hepatic (biliary obstruction).
What does pale stool and dark urine indicate?
Obstructive jaundice (conjugated bilirubin cannot reach intestines but is excreted in urine).
Can jaundice be reversed?
Yes—depending on cause: infections, stones, and some tumors are treatable.
What is Gilbert’s syndrome?
A benign condition with mild unconjugated hyperbilirubinemia due to reduced UGT1A1 activity.
When is ERCP used?
To relieve biliary obstruction and diagnose tumors or strictures in the bile duct.
Conclusion
Jaundice is not a disease but a sign of underlying pathology. Distinguishing its type through clinical signs and biochemical profiles enables targeted investigation and management—ranging from viral hepatitis to biliary obstructions and malignancy.
- Neck Lump: Causes, Diagnosis & Treatment
- Dysphagia: Causes, Diagnosis & Treatment
- Haemoptysis: Causes, Diagnosis & Treatment
- Breast Lump: Causes, Diagnosis & Treatment
- Breast Pain: Causes, Diagnosis & Treatment
- Nipple Discharge: Causes & Diagnosis
- Upper GI Bleeding: Causes & Diagnosis
- Lower GI Bleeding: Causes & Diagnosis
- Dyspepsia: Causes, Symptoms & Treatment
- Acute Abdominal Pain: Causes & Diagnosis
- Chronic Abdominal Pain: Causes & Diagnosis
- Abdominal Swelling: Causes & Diagnosis
- Upper Abdominal Swelling: Causes
- Epigastric & Umbilical Abdominal Swelling
- Lower Abdominal Swelling: Causes
- Jaundice: Causes, Types & Diagnosis (LFT)
- Diarrhoea: Causes, Types & Diagnosis
- Altered Bowel Habit & Constipation
- Groin Swelling: Causes & Diagnosis
- Claudication: Leg Pain on Walking
- Acute Warm Painful Leg: Possible Causes
- Acute Cold Leg: Causes & Emergency
- Leg Ulceration: Types & Treatment
- Dysuria: Painful Urination
- Urinary Retention: Causes & Management
- Haematuria: Blood in Urine
- Scrotal Swellings: Differential Diagnosis
- Stomas & Surgical Incisions Care
- General Anaesthesia: Principles & Risks
- Regional Anaesthesia Types & Uses
- Hypoxia: Causes, Signs & Treatment
- Surgical Infections: Prevention & Management
- Post-Op Surgical Infections: Specific Types
- Sepsis: Recognition & Urgent Treatment
- Systemic Inflammatory Response Syndrome (SIRS)
- Shock: Types & Clinical Management
- Acute Kidney Injury (AKI): Causes & Treatment
- Fractures: Types & Healing
- Congenital Childhood Orthopaedic Disorders
- Metabolic & Infective Bone Disorders
- Arthritis: Types & Management
- Musculoskeletal Tumours Overview
- Burns: Assessment & Treatment
- Major Trauma: Initial Management
- Traumatic Brain Injury: Nursing & Care
- GERD: Gastro-oesophageal Reflux Disease
- Oesophageal Carcinoma: Signs & Treatment
- Peptic Ulcer Disease (PUD)
- Gastric Carcinoma: Diagnosis & Care
- Malabsorption: Symptoms, Causes & Treatment
- Crohn’s Disease: Symptoms & Treatment
- Acute Appendicitis: Symptoms & Treatment
- Diverticular Disease: Symptoms & Treatment
- Ulcerative Colitis: Symptoms & Treatment
- Colorectal Carcinoma: Symptoms & Treatment
- Benign Anal & Perianal Disorders
- Intestinal Obstruction: Causes & Symptoms
- Abdominal Hernias: Types, Symptoms & Surgery
- Gallstone Disease: Causes & Symptoms
- Gallstone Disease: Diagnosis & Surgery
- Pancreatitis: Causes & Management
- Pancreatic Tumours: Types & Treatment
- Benign Breast Disease
- Breast Cancer: Diagnosis & Treatment
- Goitre: Causes, Symptoms & Treatment
- Thyroid Malignancies: Types & Symptoms
- Parathyroid Disease: Symptoms & Causes