General anaesthesia (GA) is a critical component of modern surgical practice, enabling patients to undergo complex procedures without awareness or pain. But what really happens from the time you enter the OT to the moment you regain consciousness?
In this guide, we break down the types of anaesthesia, pre-operative assessment, techniques used, key monitoring methods, and the innovative ERAS protocols aimed at improving recovery.
What Is General Anaesthesia?
General anaesthesia induces a controlled, reversible state of unconsciousness, with loss of sensation, muscle relaxation, and loss of reflexes. It is typically administered intravenously or via inhalation, and works by suppressing central nervous system activity.
The components of GA include:
- Analgesia (pain relief)
- Amnesia (loss of memory)
- Hypnosis (loss of consciousness)
- Muscle relaxation
Pre-operative Assessment: The First Step
Before any surgical procedure, the anaesthetist evaluates the patient to devise a safe and effective plan. This includes:
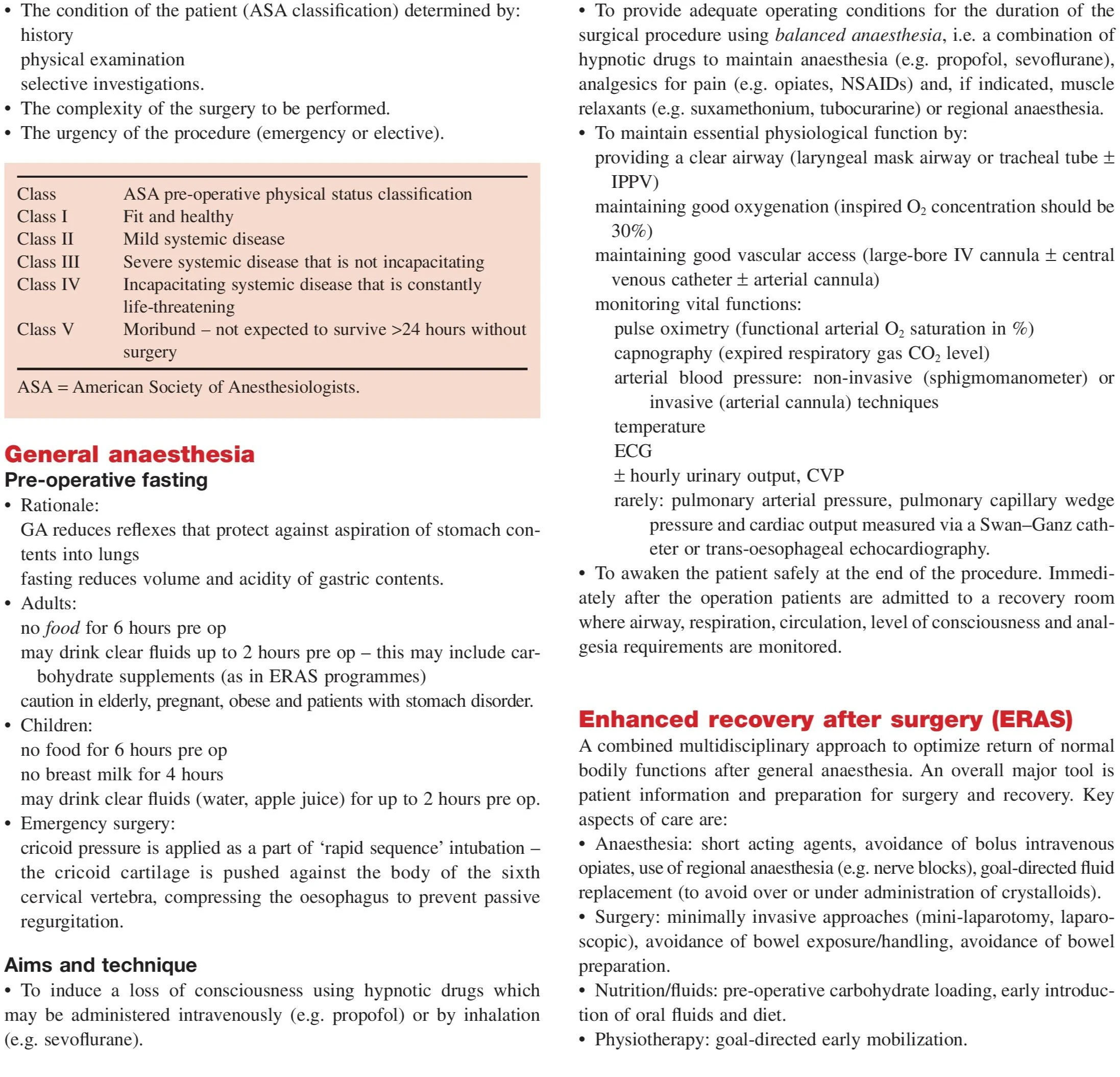
- ASA Classification (American Society of Anesthesiologists): Ranges from I (healthy) to V (moribund).
- Type of surgery: Minor, intermediate, or major.
- Urgency: Emergency vs elective.
- Health status: Including comorbidities, allergies, medications.
A detailed history, physical exam, and lab investigations help assess risk and inform anaesthetic choice.
Pre-operative Fasting Guidelines
Fasting is critical to prevent aspiration during anaesthesia. Here's how guidelines differ:
| Patient Type | Fasting Duration |
|---|---|
| Adults | No food for 6 hours, clear fluids until 2 hours prior |
| Children | Same as adults, breast milk allowed up to 4 hours prior |
| Emergency | Cricoid pressure applied during intubation to prevent aspiration |
Special considerations apply to pregnant, obese, and geriatric patients.
Induction, Maintenance & Recovery: The Anaesthetic Process
1. Induction Phase
Goal: Induce unconsciousnessMethods:
- IV drugs (e.g. Propofol, Thiopentone)
- Inhalation agents (e.g. Sevoflurane)
Airway secured via:
- Endotracheal tube
- Laryngeal mask airway
- Ventilation is initiated.
2. Maintenance Phase
Anaesthesia is maintained with:
- Inhaled gases or IV infusions
- Muscle relaxants (e.g. Succinylcholine, Vecuronium)
- Analgesics (e.g. Fentanyl, NSAIDs)
Continuous monitoring:
- ECG
- BP
- Oxygen saturation (SpO₂)
- Capnography (CO₂)
- Temperature
- Urine output
3. Recovery Phase
- Gradual withdrawal of anaesthetic agents.
- Patients regain consciousness.
- Pain is managed with pharmacological and non-pharmacological methods.
- Close monitoring in recovery room.
Balanced Anaesthesia: Combining Multiple Agents
Balanced anaesthesia aims to minimize drug side effects by combining:
- Hypnotics (to induce unconsciousness)
- Analgesics (to manage pain)
- Muscle relaxants (for surgical access)
This allows for lower doses of each agent and safer, smoother surgeries.
Monitoring Vital Functions During Anaesthesia
Key parameters are continuously observed to ensure patient safety:
| Parameter | Monitoring Tool |
|---|---|
| ECG | Heart rhythm |
| BP | Sphygmomanometer or arterial line |
| Oxygen saturation | Pulse oximeter |
| CO₂ levels | Capnograph |
| Urine output | Catheter |
| Temperature | Digital/skin probe |
| CVP (Central Venous Pressure) | Catheter line (in complex cases) |
Types of Anaesthetic Drugs Used
| Drug Type | Examples | Purpose |
|---|---|---|
| Hypnotics | Propofol, Thiopentone | Induce sleep |
| Analgesics | Fentanyl, Morphine | Pain relief |
| Muscle Relaxants | Vecuronium, Rocuronium | Reduce muscle tone |
| Inhalational agents | Sevoflurane, Isoflurane | Maintain anaesthesia |
| Anti-emetics | Ondansetron | Prevent nausea |
Regional vs General Anaesthesia: When to Choose What
Regional anaesthesia (e.g., spinal, epidural, nerve blocks) is preferred when:
- Patient is anticoagulated (GA is risky)
- Obstetrics or limb surgeries are performed
- Faster recovery and fewer complications are desired
However, general anaesthesia is necessary for:
- Major abdominal or thoracic procedures
- Long surgeries
- Uncooperative patients or children
Enhanced Recovery After Surgery (ERAS)
ERAS protocols aim to reduce hospital stay, complications, and improve recovery.
Key components include:
Anaesthesia
- Use of short-acting agents
- Regional blocks for pain control
- Avoidance of opioids when possible
Surgery
- Minimally invasive techniques (laparoscopy, mini-laparotomy)
Nutrition
- Pre-op carbohydrate loading
- Early oral fluid intake
Physiotherapy
- Early mobilization
- Lung exercises to prevent pneumonia
Common Side Effects and Complications
| Side Effect | Cause | Prevention/Management |
|---|---|---|
| Nausea/vomiting | Anaesthetic drugs | Anti-emetics |
| Sore throat | Intubation | Gentle insertion |
| Confusion | Elderly sensitivity | Adjust drug dose |
| Hypothermia | Operating room temp | Warm blankets |
| Aspiration | Inadequate fasting | Cricoid pressure |
FAQs
Q. What is the difference between general and regional anaesthesia?
General anaesthesia puts the patient completely unconscious, while regional anaesthesia numbs a specific area without loss of consciousness.
Q. Can I drink water before surgery under general anaesthesia?
Clear fluids can be taken up to 2 hours before surgery in most patients unless contraindicated.
Q. Is general anaesthesia safe?
Yes, with modern monitoring and drug combinations, GA is generally safe. Risk is minimized through thorough pre-operative assessment.
Q. How long does it take to recover from general anaesthesia?
Most people regain consciousness within minutes after surgery, but full recovery may take hours depending on the drugs used and the individual.
Conclusion: General Anaesthesia Is Safer and Smarter Today
From risk assessment to real-time monitoring and modern ERAS protocols, general anaesthesia today is far safer and more effective than ever before. A good anaesthetic plan ensures not only a pain-free operation but also a smoother, quicker recovery.
Whether you’re a student, healthcare professional, or a patient preparing for surgery, understanding how anaesthesia works empowers you to make informed, confident decisions.
- Neck Lump: Causes, Diagnosis & Treatment
- Dysphagia: Causes, Diagnosis & Treatment
- Haemoptysis: Causes, Diagnosis & Treatment
- Breast Lump: Causes, Diagnosis & Treatment
- Breast Pain: Causes, Diagnosis & Treatment
- Nipple Discharge: Causes & Diagnosis
- Upper GI Bleeding: Causes & Diagnosis
- Lower GI Bleeding: Causes & Diagnosis
- Dyspepsia: Causes, Symptoms & Treatment
- Acute Abdominal Pain: Causes & Diagnosis
- Chronic Abdominal Pain: Causes & Diagnosis
- Abdominal Swelling: Causes & Diagnosis
- Upper Abdominal Swelling: Causes
- Epigastric & Umbilical Abdominal Swelling
- Lower Abdominal Swelling: Causes
- Jaundice: Causes, Types & Diagnosis (LFT)
- Diarrhoea: Causes, Types & Diagnosis
- Altered Bowel Habit & Constipation
- Groin Swelling: Causes & Diagnosis
- Claudication: Leg Pain on Walking
- Acute Warm Painful Leg: Possible Causes
- Acute Cold Leg: Causes & Emergency
- Leg Ulceration: Types & Treatment
- Dysuria: Painful Urination
- Urinary Retention: Causes & Management
- Haematuria: Blood in Urine
- Scrotal Swellings: Differential Diagnosis
- Stomas & Surgical Incisions Care
- General Anaesthesia: Principles & Risks
- Regional Anaesthesia Types & Uses
- Hypoxia: Causes, Signs & Treatment
- Surgical Infections: Prevention & Management
- Post-Op Surgical Infections: Specific Types
- Sepsis: Recognition & Urgent Treatment
- Systemic Inflammatory Response Syndrome (SIRS)
- Shock: Types & Clinical Management
- Acute Kidney Injury (AKI): Causes & Treatment
- Fractures: Types & Healing
- Congenital Childhood Orthopaedic Disorders
- Metabolic & Infective Bone Disorders
- Arthritis: Types & Management
- Musculoskeletal Tumours Overview
- Burns: Assessment & Treatment
- Major Trauma: Initial Management
- Traumatic Brain Injury: Nursing & Care
- GERD: Gastro-oesophageal Reflux Disease
- Oesophageal Carcinoma: Signs & Treatment
- Peptic Ulcer Disease (PUD)
- Gastric Carcinoma: Diagnosis & Care
- Malabsorption: Symptoms, Causes & Treatment
- Crohn’s Disease: Symptoms & Treatment
- Acute Appendicitis: Symptoms & Treatment
- Diverticular Disease: Symptoms & Treatment
- Ulcerative Colitis: Symptoms & Treatment
- Colorectal Carcinoma: Symptoms & Treatment
- Benign Anal & Perianal Disorders
- Intestinal Obstruction: Causes & Symptoms
- Abdominal Hernias: Types, Symptoms & Surgery
- Gallstone Disease: Causes & Symptoms
- Gallstone Disease: Diagnosis & Surgery
- Pancreatitis: Causes & Management
- Pancreatic Tumours: Types & Treatment
- Benign Breast Disease
- Breast Cancer: Diagnosis & Treatment
- Goitre: Causes, Symptoms & Treatment
- Thyroid Malignancies: Types & Symptoms
- Parathyroid Disease: Symptoms & Causes