Introduction
Dyspepsia, commonly known as indigestion, affects millions globally and can signal anything from dietary discomfort to serious gastrointestinal disease. This article provides a detailed breakdown of its causes, red flags, and modern treatment strategies.
What is Dyspepsia?
- Defined as discomfort or pain in the upper abdomen
- Can present with bloating, early satiety, epigastric burning, nausea
- Often used interchangeably with “indigestion” by patients
Key Clinical Features of Dyspepsia
- Epigastric pain or discomfort
- Bloating or fullness after meals
- Early satiety
- Nausea, belching, or mild vomiting
- Sometimes associated with heartburn or regurgitation
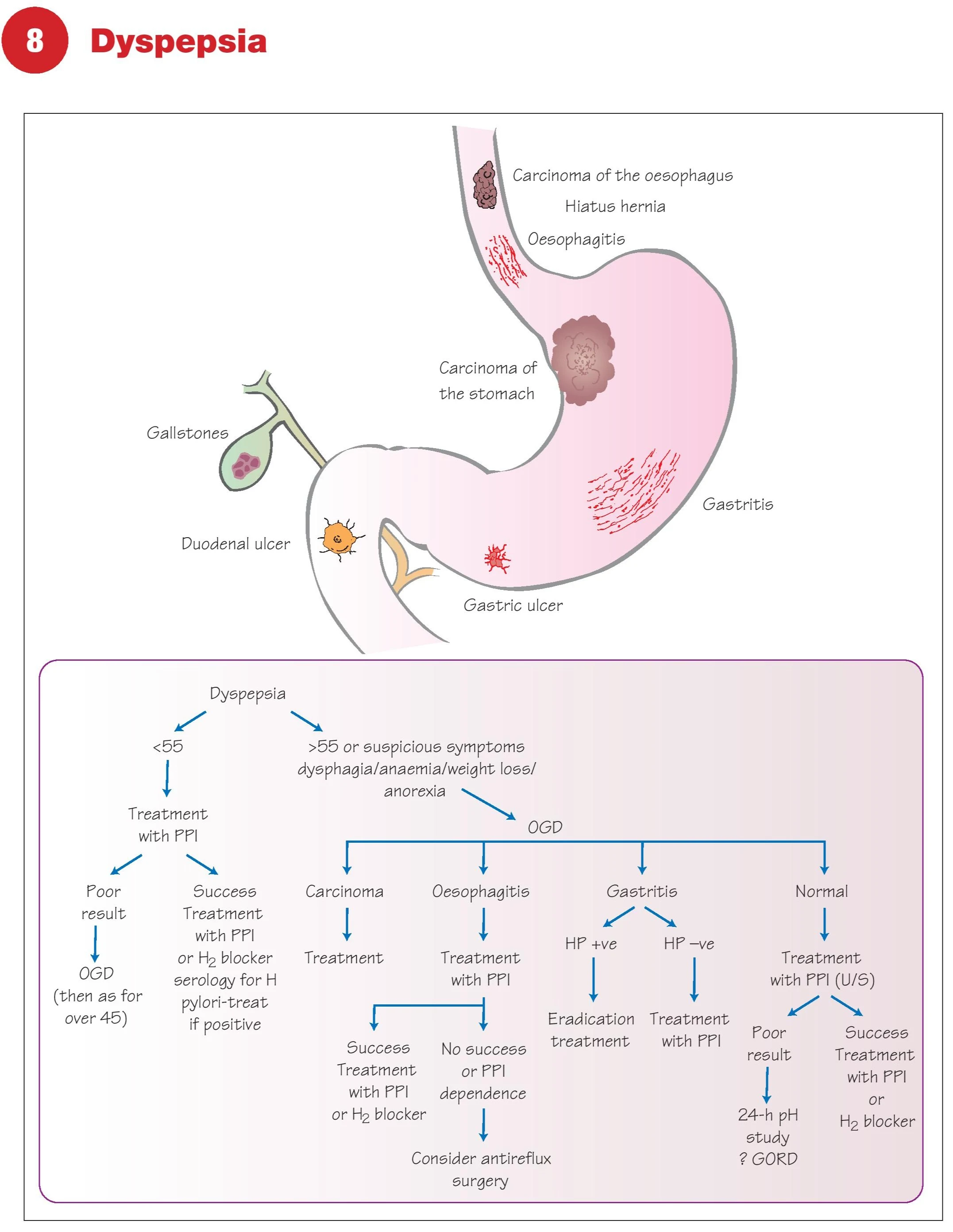
Red Flag Symptoms
- Age >55 with new symptoms
- Weight loss, anorexia
- Vomiting, anaemia
- Dysphagia or haematemesis
Any red flag warrants endoscopic evaluation (OGD)
Common Causes of Dyspepsia
1. Functional Dyspepsia
- Most common
- Normal endoscopy, unexplained symptoms
- Related to stress, slow gastric emptying
2. Gastro-oesophageal Reflux (GORD)
- Retrosternal burning, worse after meals
- Lying down worsens symptoms
- Responsive to antacids and PPIs
3. Gastritis
- Epigastric pain, transient discomfort
- May be diet or NSAID related
- Often H. pylori positive
4. Peptic Ulcer Disease (PUD)
- Gastric ulcer: worsens with food
- Duodenal ulcer: improves with food, worsens at night
- Caused by H. pylori or NSAIDs
5. Carcinoma
- Rare but serious cause
- Progressive symptoms, early satiety, weight loss, anaemia
6. Gallstones
- Not a common cause of dyspepsia alone
- Consider if RUQ pain and ultrasound positive
7. Hiatus Hernia
- Causes reflux and retrosternal pain
- May mimic dyspepsia
Differential Diagnosis of Dyspepsia
| Location | Likely Causes |
|---|---|
| Oesophagus | Reflux, oesophagitis, carcinoma |
| Stomach | Gastritis, ulcers, carcinoma |
| Duodenum | Duodenal ulcer |
| Gallbladder | Gallstones |
| Functional | Non-ulcer dyspepsia |
Diagnostic Approach to Dyspepsia
Age <55 without Alarm Symptoms
- Trial of PPI or H2 blocker
- If response: continue
- If no response: test for H. pylori → treat if positive
- If still unresponsive: proceed to endoscopy
Age >55 or with Alarm Symptoms
- Immediate OGD (endoscopy)
- Biopsy for malignancy or H. pylori
- Evaluate for gastric/oesophageal cancer, ulcers
Key Investigations
- FBC – anemia suggests malignancy
- H. pylori testing – breath test, stool antigen, serology, or biopsy CLO test
- OGD (endoscopy) – gold standard for dyspepsia with red flags
- 24-hour pH study – if GORD suspected but not confirmed
- Oesophageal manometry – for motility disorders
- Ultrasound – to rule out gallstones
Treatment Guidelines for Dyspepsia
Step 1: Empirical Therapy (Age <55)
- Start with PPI (4–8 weeks)
- If successful → continue
- If not, test and treat H. pylori
Step 2: H. pylori Eradication
- Triple therapy: PPI + 2 antibiotics (amoxicillin + clarithromycin/metronidazole)
- Reassess symptoms post-eradication
Step 3: Endoscopic Findings
- Carcinoma – Refer for cancer management
- Ulcers – Continue PPI ± eradicate H. pylori
- Oesophagitis – Long-term acid suppression
- Normal – Reassure or manage functional dyspepsia
Step 4: Functional Dyspepsia
- Reassurance, lifestyle changes
- Avoid NSAIDs, caffeine, spicy food
- Antidepressants in select cases
Lifestyle Modifications
- Smaller, more frequent meals
- Elevate head of bed if reflux
- Avoid alcohol, smoking
- Reduce fatty, spicy foods
- Manage stress and anxiety
FAQs About Dyspepsia
Is dyspepsia the same as acid reflux?
Not exactly. Reflux is one cause of dyspepsia but not the only one.
When should I worry about dyspepsia?
If you're over 55 or have red flag symptoms like weight loss or anaemia.
Can stress cause dyspepsia?
Yes. Functional dyspepsia is often worsened by stress and anxiety.
How is H. pylori diagnosed?
Via breath test, stool test, blood serology, or endoscopic biopsy.
What is the best treatment for dyspepsia?
Depends on the cause—PPI therapy is first-line, followed by eradication of H. pylori if present.
Conclusion
Dyspepsia is common, usually benign, but sometimes serious. Differentiating between functional causes and sinister pathology like ulcers or cancer is vital. With proper evaluation and treatment, most cases can be managed successfully and non-invasively.
- Neck Lump: Causes, Diagnosis & Treatment
- Dysphagia: Causes, Diagnosis & Treatment
- Haemoptysis: Causes, Diagnosis & Treatment
- Breast Lump: Causes, Diagnosis & Treatment
- Breast Pain: Causes, Diagnosis & Treatment
- Nipple Discharge: Causes & Diagnosis
- Upper GI Bleeding: Causes & Diagnosis
- Lower GI Bleeding: Causes & Diagnosis
- Dyspepsia: Causes, Symptoms & Treatment
- Acute Abdominal Pain: Causes & Diagnosis
- Chronic Abdominal Pain: Causes & Diagnosis
- Abdominal Swelling: Causes & Diagnosis
- Upper Abdominal Swelling: Causes
- Epigastric & Umbilical Abdominal Swelling
- Lower Abdominal Swelling: Causes
- Jaundice: Causes, Types & Diagnosis (LFT)
- Diarrhoea: Causes, Types & Diagnosis
- Altered Bowel Habit & Constipation
- Groin Swelling: Causes & Diagnosis
- Claudication: Leg Pain on Walking
- Acute Warm Painful Leg: Possible Causes
- Acute Cold Leg: Causes & Emergency
- Leg Ulceration: Types & Treatment
- Dysuria: Painful Urination
- Urinary Retention: Causes & Management
- Haematuria: Blood in Urine
- Scrotal Swellings: Differential Diagnosis
- Stomas & Surgical Incisions Care
- General Anaesthesia: Principles & Risks
- Regional Anaesthesia Types & Uses
- Hypoxia: Causes, Signs & Treatment
- Surgical Infections: Prevention & Management
- Post-Op Surgical Infections: Specific Types
- Sepsis: Recognition & Urgent Treatment
- Systemic Inflammatory Response Syndrome (SIRS)
- Shock: Types & Clinical Management
- Acute Kidney Injury (AKI): Causes & Treatment
- Fractures: Types & Healing
- Congenital Childhood Orthopaedic Disorders
- Metabolic & Infective Bone Disorders
- Arthritis: Types & Management
- Musculoskeletal Tumours Overview
- Burns: Assessment & Treatment
- Major Trauma: Initial Management
- Traumatic Brain Injury: Nursing & Care
- GERD: Gastro-oesophageal Reflux Disease
- Oesophageal Carcinoma: Signs & Treatment
- Peptic Ulcer Disease (PUD)
- Gastric Carcinoma: Diagnosis & Care
- Malabsorption: Symptoms, Causes & Treatment
- Crohn’s Disease: Symptoms & Treatment
- Acute Appendicitis: Symptoms & Treatment
- Diverticular Disease: Symptoms & Treatment
- Ulcerative Colitis: Symptoms & Treatment
- Colorectal Carcinoma: Symptoms & Treatment
- Benign Anal & Perianal Disorders
- Intestinal Obstruction: Causes & Symptoms
- Abdominal Hernias: Types, Symptoms & Surgery
- Gallstone Disease: Causes & Symptoms
- Gallstone Disease: Diagnosis & Surgery
- Pancreatitis: Causes & Management
- Pancreatic Tumours: Types & Treatment
- Benign Breast Disease
- Breast Cancer: Diagnosis & Treatment
- Goitre: Causes, Symptoms & Treatment
- Thyroid Malignancies: Types & Symptoms
- Parathyroid Disease: Symptoms & Causes