What Is an Acute Cold Leg?
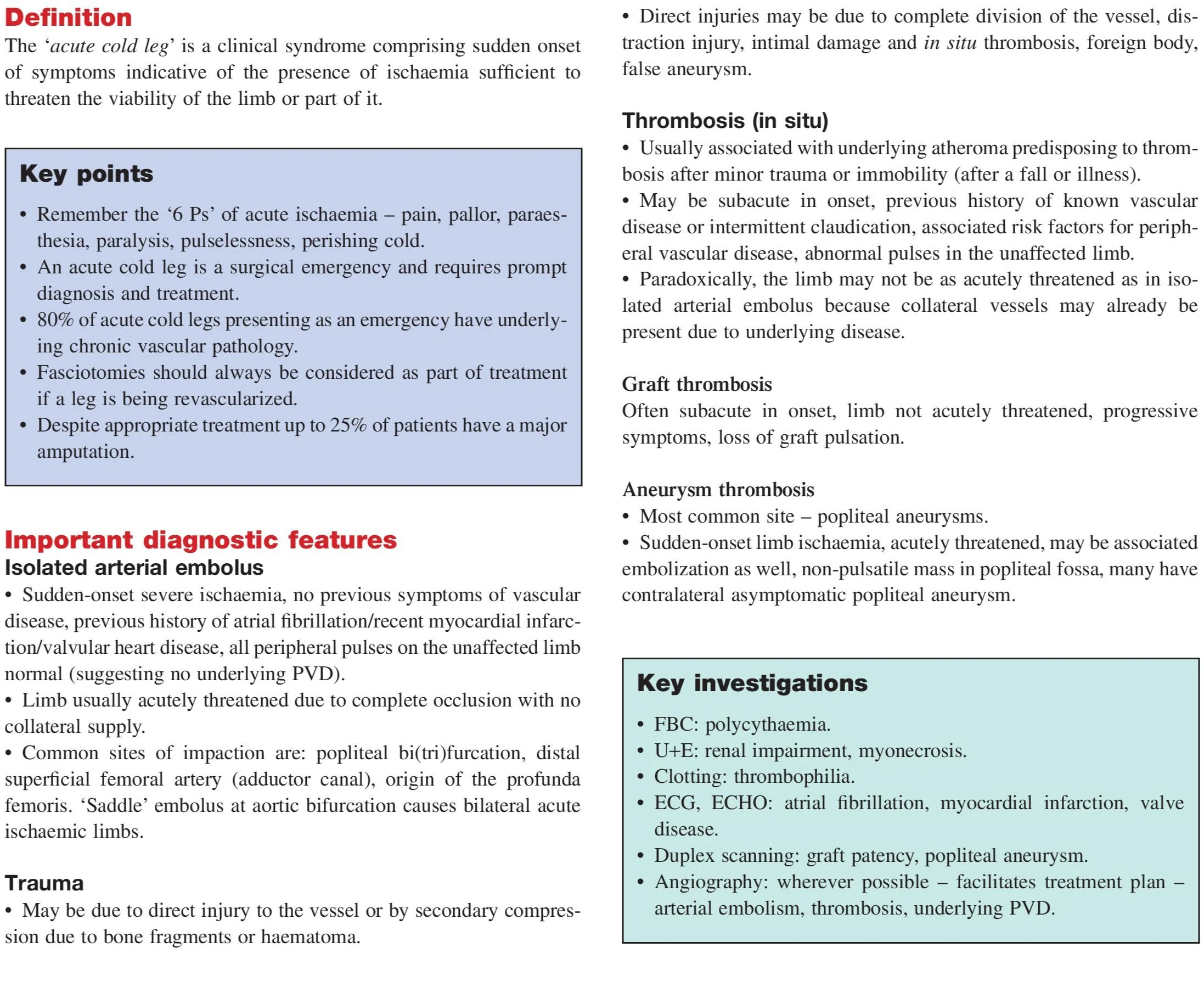
An acute cold leg is a vascular emergency marked by the sudden onset of limb ischemia, which can severely threaten the viability of the limb. It represents an abrupt cessation of arterial blood flow, commonly due to an embolus or thrombosis, leading to a classic set of symptoms known as the 6 P’s: Pain, Pallor, Pulselessness, Paresthesia, Paralysis, and Perishing cold. Prompt recognition and intervention are essential to salvage the limb and prevent mortality or amputation.
Understanding the Urgency
Acute limb ischemia (ALI) is a time-sensitive condition. Once blood flow is critically reduced, tissue hypoxia rapidly sets in. If left untreated, irreversible tissue damage can occur within 6 hours. Studies indicate that despite optimal treatment, up to 25% of patients may still undergo major amputation, and the mortality rate remains high.
Causes of Acute Cold Leg
Embolic Causes (Pure Acute)
- Atrial Fibrillation (AF) – causes mural thrombi in the heart, which embolize to limb arteries.
- Myocardial Infarction – thrombus formation in ventricular walls.
- Valvular Heart Disease – can lead to embolic episodes.
- Proximal Atheroma – unstable plaques that shed emboli.
Traumatic Causes
- Blunt trauma – direct damage to the vessel.
- Penetrating injuries – such as stab or gunshot wounds.
- Pressure/compression – due to fracture fragments or hematoma.
Acute-on-Chronic Causes
- Thrombosis of Atherosclerotic Plaques – especially in patients with intermittent claudication or known peripheral vascular disease.
- Thrombosis of Popliteal Aneurysm – most common site of aneurysmal thrombosis.
- Graft Thrombosis – failure of a previously placed vascular graft.
Classification: Pure Acute vs Acute on Chronic
- Pure Acute: Caused by embolism, in patients without prior vascular symptoms. Contralateral pulses are usually normal.
- Acute on Chronic: Thrombosis on pre-existing atherosclerotic vessels. Often subacute with progressive symptoms. Contralateral limb shows signs of vascular disease.
Clinical Assessment and Diagnosis
Clinical Features by Limb Viability:
- Viable (Chronically Threatened): Rest pain, preserved motor/sensory function.
- Acutely Threatened: Rest pain + sensory loss ± motor loss.
- Non-Viable: Fixed staining, woody muscles, and long-standing ischemia.
Diagnostic Features:
- Embolism: Sudden onset, no prior claudication, AF/MI history, normal pulses in other limb.
- Thrombosis: History of vascular disease or trauma, abnormal contralateral pulses.
Key Investigations
- FBC: To rule out polycythemia
- U+E: Evaluate renal function and myonecrosis
- Clotting profile: Thrombophilia screen
- ECG/ECHO: Detect AF, MI, or valvular lesions
- Duplex Scan: Check for graft patency, aneurysms
- Angiography: Gold standard to identify site and nature of occlusion
Emergency Management Algorithm
- Initial Step: Start IV unfractionated heparin
- Assessment: Clinical + Doppler exam
- Determine Cause: ECG, Echo, Angiography, U/S
Treatment Options
Leg Viable (Chronically Threatened)
- Formal angiography
- Catheter-Directed Thrombolysis (CDT)
- Percutaneous Mechanical Thrombectomy (PMT)
- Angioplasty ± Stent
- Embolectomy ± Bypass Surgery
Leg Acutely Threatened
Immediate Treatment:
- CDT or PMT
- Angioplasty ± stenting
- Surgery (embolectomy ± bypass)
- ± Fasciotomy for compartment syndrome
Leg Non-Viable
- Primary Amputation
- If in a terminal stage, palliative care is advised
Surgical and Endovascular Options
- Catheter-Directed Thrombolysis (CDT): Effective for fresh thrombi
- Mechanical Aspiration (PMT): Minimally invasive removal of clot
- Angioplasty/Stenting: Restores vessel patency
- Surgical Embolectomy: Balloon catheter removal of embolus
- Fasciotomy: Prevents reperfusion injury in prolonged ischemia
Prognosis and Recurrence
- Prognosis depends on the speed of intervention and underlying pathology
- Recurrence is high in untreated chronic vascular disease
- Long-term anticoagulation, lifestyle changes, and secondary prevention crucial
Prevention of Acute Limb Ischemia
- Manage AF: Use anticoagulants (e.g., warfarin, DOACs)
- Control Risk Factors: Diabetes, hypertension, smoking
- Surveillance: Post-bypass grafts and known aneurysms
- Exercise and Diet: Prevent progression of atherosclerosis
Conclusion
Acute cold leg is a vascular emergency that demands rapid recognition and immediate action. Delays in diagnosis or management can result in irreversible tissue damage, amputation, or death. Recognizing the 6 Ps, initiating heparin promptly, classifying limb viability accurately, and choosing the right interventional approach are key to saving limbs and lives.
- Neck Lump: Causes, Diagnosis & Treatment
- Dysphagia: Causes, Diagnosis & Treatment
- Haemoptysis: Causes, Diagnosis & Treatment
- Breast Lump: Causes, Diagnosis & Treatment
- Breast Pain: Causes, Diagnosis & Treatment
- Nipple Discharge: Causes & Diagnosis
- Upper GI Bleeding: Causes & Diagnosis
- Lower GI Bleeding: Causes & Diagnosis
- Dyspepsia: Causes, Symptoms & Treatment
- Acute Abdominal Pain: Causes & Diagnosis
- Chronic Abdominal Pain: Causes & Diagnosis
- Abdominal Swelling: Causes & Diagnosis
- Upper Abdominal Swelling: Causes
- Epigastric & Umbilical Abdominal Swelling
- Lower Abdominal Swelling: Causes
- Jaundice: Causes, Types & Diagnosis (LFT)
- Diarrhoea: Causes, Types & Diagnosis
- Altered Bowel Habit & Constipation
- Groin Swelling: Causes & Diagnosis
- Claudication: Leg Pain on Walking
- Acute Warm Painful Leg: Possible Causes
- Acute Cold Leg: Causes & Emergency
- Leg Ulceration: Types & Treatment
- Dysuria: Painful Urination
- Urinary Retention: Causes & Management
- Haematuria: Blood in Urine
- Scrotal Swellings: Differential Diagnosis
- Stomas & Surgical Incisions Care
- General Anaesthesia: Principles & Risks
- Regional Anaesthesia Types & Uses
- Hypoxia: Causes, Signs & Treatment
- Surgical Infections: Prevention & Management
- Post-Op Surgical Infections: Specific Types
- Sepsis: Recognition & Urgent Treatment
- Systemic Inflammatory Response Syndrome (SIRS)
- Shock: Types & Clinical Management
- Acute Kidney Injury (AKI): Causes & Treatment
- Fractures: Types & Healing
- Congenital Childhood Orthopaedic Disorders
- Metabolic & Infective Bone Disorders
- Arthritis: Types & Management
- Musculoskeletal Tumours Overview
- Burns: Assessment & Treatment
- Major Trauma: Initial Management
- Traumatic Brain Injury: Nursing & Care
- GERD: Gastro-oesophageal Reflux Disease
- Oesophageal Carcinoma: Signs & Treatment
- Peptic Ulcer Disease (PUD)
- Gastric Carcinoma: Diagnosis & Care
- Malabsorption: Symptoms, Causes & Treatment
- Crohn’s Disease: Symptoms & Treatment
- Acute Appendicitis: Symptoms & Treatment
- Diverticular Disease: Symptoms & Treatment
- Ulcerative Colitis: Symptoms & Treatment
- Colorectal Carcinoma: Symptoms & Treatment
- Benign Anal & Perianal Disorders
- Intestinal Obstruction: Causes & Symptoms
- Abdominal Hernias: Types, Symptoms & Surgery
- Gallstone Disease: Causes & Symptoms
- Gallstone Disease: Diagnosis & Surgery
- Pancreatitis: Causes & Management
- Pancreatic Tumours: Types & Treatment
- Benign Breast Disease
- Breast Cancer: Diagnosis & Treatment
- Goitre: Causes, Symptoms & Treatment
- Thyroid Malignancies: Types & Symptoms
- Parathyroid Disease: Symptoms & Causes