Intestinal obstruction is a serious and potentially life-threatening condition that occurs when the normal flow of intestinal contents is blocked. It can affect the small intestine, large intestine, or both and may be mechanical (physical blockage) or functional (paralysis of intestinal muscles). Timely recognition and management are crucial to avoid complications like ischemia, necrosis, and perforation.
This guide explains everything you need to know — from the pathophysiology and symptoms to diagnosis and modern treatment protocols — in a structured, medically accurate, and reader-friendly format.
What is Intestinal Obstruction?
Intestinal obstruction refers to the partial or complete blockage of the bowel that prevents food, fluids, and gas from moving through the intestines. It can be:
Complete vs. Incomplete: Total vs. partial blockage
Acute vs. Chronic: Hours to days vs. weeks- Simple: No blood supply compromise
- Strangulated: Blood flow is impaired → ischemia, gangrene
Key Points
- Small bowel obstruction (SBO): Rapid onset, often due to adhesions or hernias
- Large bowel obstruction (LBO): Gradual onset, often from carcinoma or volvulus
- Dehydration and electrolyte loss are common complications
- Prompt diagnosis and fluid replacement are critical
- Surgery is often needed if conservative measures fail
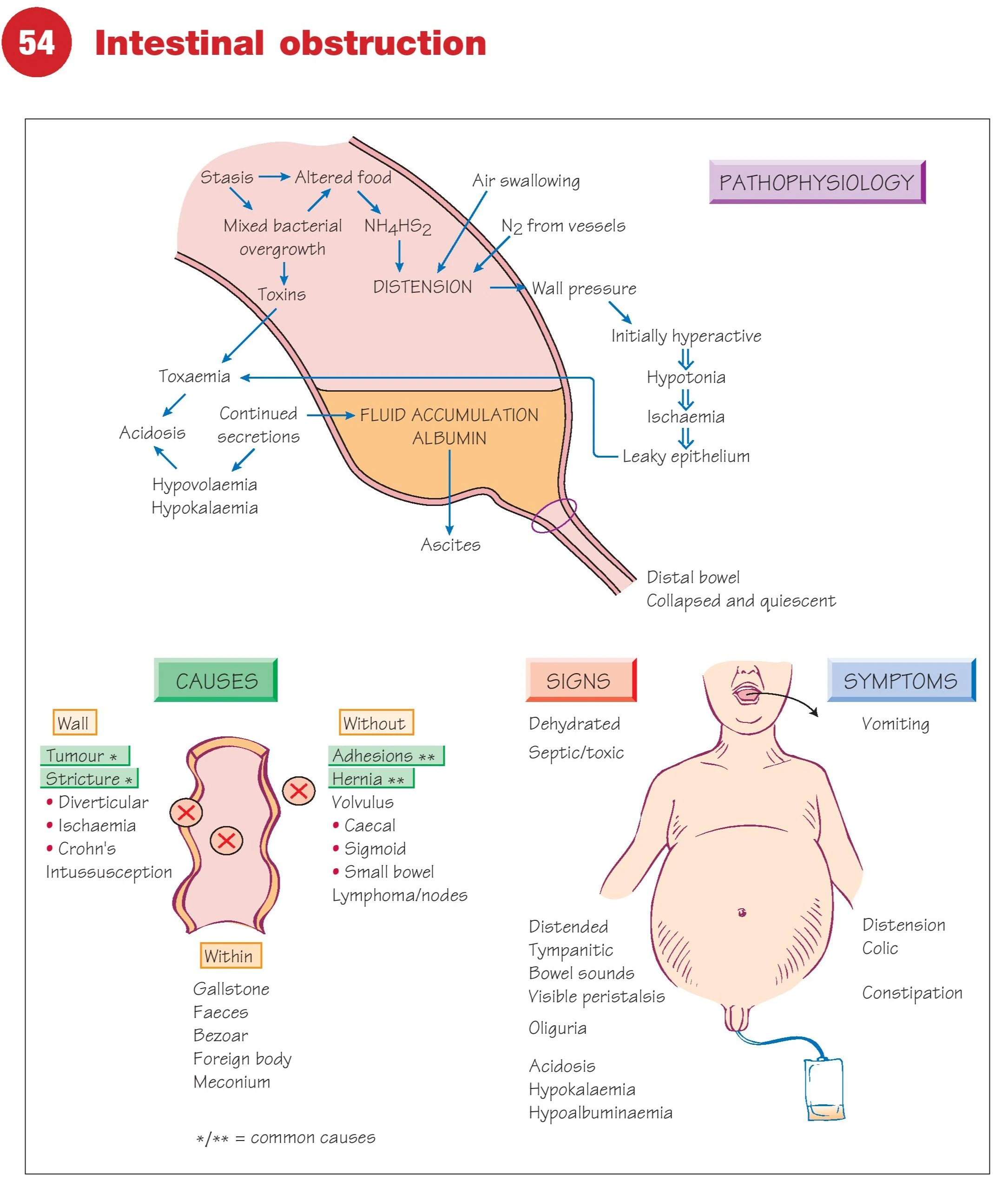
Causes of Intestinal Obstruction
Mechanical Causes
1. Within the Bowel Lumen:
- Gallstones
- Fecal impaction
- Bezoars
- Foreign bodies
- Meconium (neonates)
2. Within the Bowel Wall:
- Tumors (adenocarcinoma, lymphoma)
- Strictures (Crohn’s disease, diverticulitis)
- Ischemia
- Intussusception
3. External Compression:
- Adhesions (post-surgery)
- Hernias (inguinal, femoral, incisional)
- Volvulus (sigmoid, cecal)
- Bands and tumors compressing the bowel
Functional (Paralytic/Adynamic Ileus):
- Surgery
- Trauma
- Sepsis
- Electrolyte disturbances (especially low potassium)
- Drugs (opioids, anticholinergics)
Pathophysiology
Obstruction leads to:
- Proximal bowel distension → fluid, gas accumulation
- Bacterial overgrowth and toxin production
- Venous congestion and wall edema
- Compromised blood flow → ischemia → necrosis → perforation
- Loss of fluid into bowel lumen → dehydration, hypovolemia
- Electrolyte imbalance → acidosis, hypokalemia, hypoalbuminemia
Common Types by Location
Small Bowel Obstruction (SBO)
| Segment | Common Causes |
|---|---|
| Duodenum | Pancreatic or duodenal tumors, ulcers |
| Jejunum/Ileum | Adhesions, hernias, Crohn’s, tumors, FBs |
| Neonates | Meconium ileus, atresia, volvulus |
Large Bowel Obstruction (LBO)
| Location | Common Causes |
|---|---|
| Colon | Tumors, diverticulitis, volvulus, fecaloma |
| Neonates | Hirschsprung’s disease, atresia |
Symptoms of Intestinal Obstruction
- Vomiting: Early in SBO, late or absent in LBO
- Abdominal distension
- Colicky abdominal pain
- Absolute constipation: No gas or stool passage
- Visible peristalsis
- Borborygmi (hyperactive sounds) in early stages, absent later
- Oliguria: Reduced urine output
- Signs of dehydration: Dry tongue, low BP
- Tympanic abdomen
Signs of Complicated Obstruction
- Fever, tachycardia
- Localized tenderness or guarding → possible ischemia or perforation
- Empty rectum on digital exam
- Shock (due to sepsis or fluid loss)
Investigations
Bedside and Lab Tests:
Blood tests:
- CBC: Hemoconcentration, leukocytosis
- U&E: Hypokalemia, uremia
- CRP/ESR: Inflammation
Imaging:
Abdominal X-ray:
- Dilated bowel loops
- Air-fluid levels
- Ladder-like pattern (SBO)
- Large bowel: ‘Coffee bean’ sign in volvulus
CT Scan (Gold Standard):
- Site and cause of obstruction
- Closed-loop, strangulated, or ischemic bowel
Ultrasound (especially in children)
Barium Enema: For large bowel obstruction
Sigmoidoscopy: In suspected sigmoid volvulusManagement of Intestinal Obstruction
Initial Resuscitation
- NPO (nil per os): Nothing by mouth
- NG tube: To decompress stomach
- IV fluids: Correct hypovolemia, electrolyte balance
- Antibiotics: If perforation/ischemia suspected
- Analgesia: Avoid masking signs of peritonitis
Conservative Management (When Stable)
- Adhesions (initial attempt)
- Partial SBO without peritonitis
- Monitor with serial exams, input/output charting, abdominal girth
- Repeat imaging in 12–24 hours
Surgical Intervention
Indications:
- Strangulation suspected
- Perforation signs
- Incomplete response to conservative treatment
- Mechanical cause (tumor, hernia, volvulus)
Common Procedures:
| Cause | Surgery |
|---|---|
| Adhesions | Adhesiolysis |
| Hernia | Hernia repair ± bowel resection |
| Tumor | Resection (e.g., right hemicolectomy) |
| Volvulus (Sigmoid) | Decompression ± resection |
| Intussusception | Reduction or resection (adults) |
| Ischemia | Resection of gangrenous segment |
Complications of Untreated Obstruction
- Bowel perforation
- Sepsis
- Peritonitis
- Electrolyte imbalance (life-threatening)
- Short bowel syndrome (if large segments are removed)
- Death (especially in elderly with comorbidities)
Prevention
- Timely surgery for hernias and tumors
- Post-op care to prevent adhesions
- Hydration and mobility after abdominal surgery
- Dietary fiber for healthy bowel habits
- Avoid narcotics and constipating medications in at-risk patients
Summary Table: Intestinal Obstruction at a Glance
| Feature | Small Bowel Obstruction | Large Bowel Obstruction |
|---|---|---|
| Common Onset | Acute | Gradual |
| Common Causes | Adhesions, hernia | Tumors, volvulus |
| Vomiting | Prominent | Late or absent |
| Abdominal Distension | Mild to moderate | Marked |
| Bowel Sounds | Hyperactive early, then absent | Dull or absent |
| Diagnosis | X-ray, CT | CT, sigmoidoscopy, enema |
| Management | Conservative ± surgery | Usually surgical |
FAQs
Q1: How long can intestinal obstruction last without surgery?
A: Partial obstructions may resolve with conservative treatment. Complete obstructions or those with ischemia require urgent surgery.
Q2: Is intestinal obstruction life-threatening?
A: Yes, if not treated. It can lead to necrosis, perforation, and sepsis.
Q3: Can constipation cause intestinal obstruction?
A: Severe fecal impaction can mimic or cause obstruction, especially in the elderly.
Q4: What foods to avoid post-obstruction?
A: Avoid high-fiber and gas-producing foods initially. Resume normal diet gradually under supervision.
Q5: How is bowel function restored after obstruction?
A: Through decompression, hydration, and careful reintroduction of oral intake. Surgery may restore function if part of the bowel is removed.
- Neck Lump: Causes, Diagnosis & Treatment
- Dysphagia: Causes, Diagnosis & Treatment
- Haemoptysis: Causes, Diagnosis & Treatment
- Breast Lump: Causes, Diagnosis & Treatment
- Breast Pain: Causes, Diagnosis & Treatment
- Nipple Discharge: Causes & Diagnosis
- Upper GI Bleeding: Causes & Diagnosis
- Lower GI Bleeding: Causes & Diagnosis
- Dyspepsia: Causes, Symptoms & Treatment
- Acute Abdominal Pain: Causes & Diagnosis
- Chronic Abdominal Pain: Causes & Diagnosis
- Abdominal Swelling: Causes & Diagnosis
- Upper Abdominal Swelling: Causes
- Epigastric & Umbilical Abdominal Swelling
- Lower Abdominal Swelling: Causes
- Jaundice: Causes, Types & Diagnosis (LFT)
- Diarrhoea: Causes, Types & Diagnosis
- Altered Bowel Habit & Constipation
- Groin Swelling: Causes & Diagnosis
- Claudication: Leg Pain on Walking
- Acute Warm Painful Leg: Possible Causes
- Acute Cold Leg: Causes & Emergency
- Leg Ulceration: Types & Treatment
- Dysuria: Painful Urination
- Urinary Retention: Causes & Management
- Haematuria: Blood in Urine
- Scrotal Swellings: Differential Diagnosis
- Stomas & Surgical Incisions Care
- General Anaesthesia: Principles & Risks
- Regional Anaesthesia Types & Uses
- Hypoxia: Causes, Signs & Treatment
- Surgical Infections: Prevention & Management
- Post-Op Surgical Infections: Specific Types
- Sepsis: Recognition & Urgent Treatment
- Systemic Inflammatory Response Syndrome (SIRS)
- Shock: Types & Clinical Management
- Acute Kidney Injury (AKI): Causes & Treatment
- Fractures: Types & Healing
- Congenital Childhood Orthopaedic Disorders
- Metabolic & Infective Bone Disorders
- Arthritis: Types & Management
- Musculoskeletal Tumours Overview
- Burns: Assessment & Treatment
- Major Trauma: Initial Management
- Traumatic Brain Injury: Nursing & Care
- GERD: Gastro-oesophageal Reflux Disease
- Oesophageal Carcinoma: Signs & Treatment
- Peptic Ulcer Disease (PUD)
- Gastric Carcinoma: Diagnosis & Care
- Malabsorption: Symptoms, Causes & Treatment
- Crohn’s Disease: Symptoms & Treatment
- Acute Appendicitis: Symptoms & Treatment
- Diverticular Disease: Symptoms & Treatment
- Ulcerative Colitis: Symptoms & Treatment
- Colorectal Carcinoma: Symptoms & Treatment
- Benign Anal & Perianal Disorders
- Intestinal Obstruction: Causes & Symptoms
- Abdominal Hernias: Types, Symptoms & Surgery
- Gallstone Disease: Causes & Symptoms
- Gallstone Disease: Diagnosis & Surgery
- Pancreatitis: Causes & Management
- Pancreatic Tumours: Types & Treatment
- Benign Breast Disease
- Breast Cancer: Diagnosis & Treatment
- Goitre: Causes, Symptoms & Treatment
- Thyroid Malignancies: Types & Symptoms
- Parathyroid Disease: Symptoms & Causes