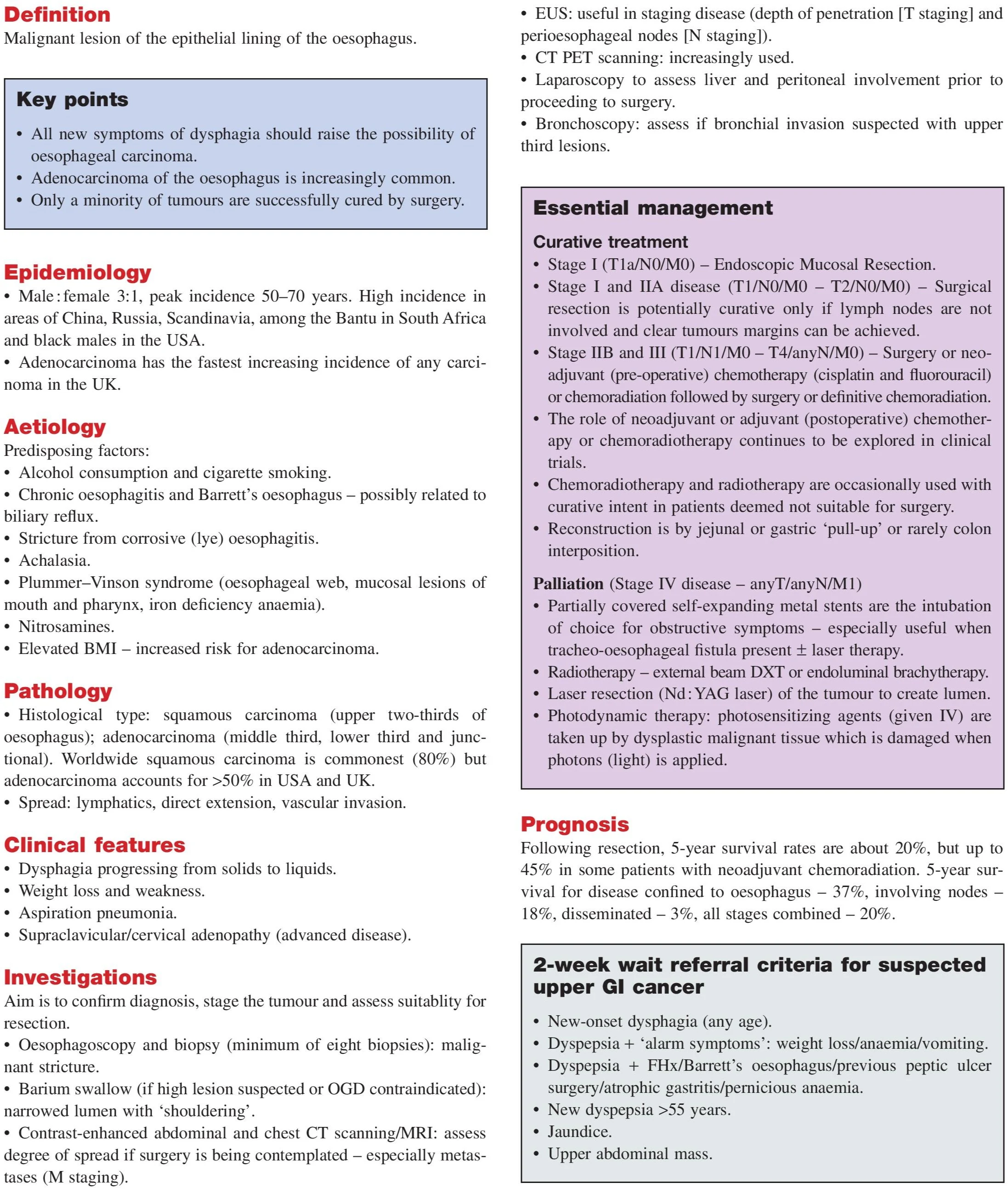
Oesophageal carcinoma is a malignant tumor of the epithelial lining of the oesophagus. It presents most commonly with progressive dysphagia and can spread rapidly due to its close proximity to major structures and lymphatic channels.
Key Facts and Epidemiology
- Male:Female ratio = 3:1
- Peak incidence: 50–70 years
- High-risk areas: China, Russia, Scandinavia, South Africa (Bantu population), USA (Black males)
- Adenocarcinoma is rising fast in Western countries due to Barrett’s oesophagus
Causes and Risk Factors (Aetiology)
Predisposing Conditions:
- Chronic alcohol and tobacco use
- Barrett’s oesophagus (GORD-related)
- Achalasia (failure of LOS to relax)
- Lye (caustic) strictures from corrosive ingestion
- Plummer–Vinson syndrome
- Nitrosamines (dietary carcinogens)
- High BMI (especially for adenocarcinoma)
Types of Oesophageal Cancer
By Morphology:
- Malignant stricture
- Malignant ulcer
- Invasive mass
- Carcinoma in Barrett’s oesophagus
By Histology:
- Squamous cell carcinoma (80% worldwide, upper 2/3)
- Adenocarcinoma (lower 1/3 and junctional – 50% in UK/USA)
How Oesophageal Cancer Spreads (as per diagram)
Local invasion: trachea, lung, aorta
Lymphatic spread:
- Supraclavicular (Virchow’s node)
- Mediastinal nodes
- Gastric nodes
Distant metastases: liver, bone, lung
Symptoms due to spread:
- Dysphagia
- Haemoptysis
- Cough
- Dyspnoea
- Dyspepsia
- Pleural and pericardial effusion
Clinical Symptoms and Red Flags
- Progressive dysphagia (solids → liquids)
- Odynophagia (painful swallowing)
- Weight loss
- Hoarseness or cough (nerve involvement)
- Aspiration pneumonia
- Retrosternal chest pain or epigastric pain
- Cervical lymphadenopathy (advanced disease)
TNM Staging of Oesophageal Cancer (as per diagram)
T – Tumor Invasion:
- Tis: in situ
- T1a/T1b: mucosa/submucosa
- T2: muscularis propria
- T3: adventitia
- T4a/T4b: adjacent organs (lung, bone, etc.)
N – Nodes:
- N0: no nodes
- N1: 1–2 nodes
- N2: 3–6 nodes
- N3: ≥7 nodes
M – Metastasis:
- M0: no metastasis
- M1: distant metastasis
How It’s Diagnosed: Investigations
Initial tests:
- OGD + biopsy (gold standard)
- Barium swallow – assesses obstruction, fistula, or stricture
- CT Chest/Abdomen – stage and assess resectability
- Endoscopic Ultrasound (EUS) – evaluate local invasion
- PET-CT – detects distant spread
- Laparoscopy – assess peritoneal involvement
- Bronchoscopy – assess tracheobronchial invasion (if upper third)
Pathology and Histological Types
- Squamous cell carcinoma: upper/middle oesophagus
- Adenocarcinoma: lower third and gastro-oesophageal junction
- Spread: lymphatic, submucosal, vascular
Surgical Options by Tumor Site (Diagram-Based)
Lower 1/3 or Junctional
- Total gastrectomy + Roux-en-Y
- Oesophago-gastrectomy
Upper 1/3
- Oesophagectomy + interposition graft
Postcricoid tumors
- Pharyngo-laryngo-oesophagectomy + interposition graft
Treatment by Stage: Curative vs Palliative
Curative Options
- Stage Tis/T1a: Endoscopic mucosal resection
- Stage I/IIA: Surgery if margins are clear and no node involvement
- Stage IIB/III: Chemoradiation + surgery or definitive chemoradiation
- Reconstruction: Gastric pull-up or colon interposition
Palliative Options
- Metal stents – relieve obstruction
- Radiotherapy – DXT or brachytherapy
- Laser/YAG debulking
- Photodynamic therapy – destroys dysplastic cells
Prognosis and Survival Rates
Post-surgical 5-year survival: ~20%
With neoadjuvant chemoradiation: up to 45%
Survival by extent:
- Local: 37%
- Node-positive: 18%
- Disseminated: 3%
- Overall: 20%
Frequently Asked Questions (FAQs)
Q1. What is the most common symptom of oesophageal carcinoma?
Progressive dysphagia – difficulty swallowing solids first, then liquids.
Q2. Can Barrett’s oesophagus cause cancer?
Yes. Adenocarcinoma arising in Barrett’s is increasingly common, especially in Western countries.
Q3. What is the difference between squamous and adenocarcinoma of the oesophagus?
-
Squamous: upper/mid part, linked to smoking/alcohol
-
Adenocarcinoma: lower oesophagus, often from Barrett’s
Q4. Is surgery always possible for oesophageal cancer?
No. Advanced/metastatic tumors may not be resectable. Palliative care is needed in such cases.
- Neck Lump: Causes, Diagnosis & Treatment
- Dysphagia: Causes, Diagnosis & Treatment
- Haemoptysis: Causes, Diagnosis & Treatment
- Breast Lump: Causes, Diagnosis & Treatment
- Breast Pain: Causes, Diagnosis & Treatment
- Nipple Discharge: Causes & Diagnosis
- Upper GI Bleeding: Causes & Diagnosis
- Lower GI Bleeding: Causes & Diagnosis
- Dyspepsia: Causes, Symptoms & Treatment
- Acute Abdominal Pain: Causes & Diagnosis
- Chronic Abdominal Pain: Causes & Diagnosis
- Abdominal Swelling: Causes & Diagnosis
- Upper Abdominal Swelling: Causes
- Epigastric & Umbilical Abdominal Swelling
- Lower Abdominal Swelling: Causes
- Jaundice: Causes, Types & Diagnosis (LFT)
- Diarrhoea: Causes, Types & Diagnosis
- Altered Bowel Habit & Constipation
- Groin Swelling: Causes & Diagnosis
- Claudication: Leg Pain on Walking
- Acute Warm Painful Leg: Possible Causes
- Acute Cold Leg: Causes & Emergency
- Leg Ulceration: Types & Treatment
- Dysuria: Painful Urination
- Urinary Retention: Causes & Management
- Haematuria: Blood in Urine
- Scrotal Swellings: Differential Diagnosis
- Stomas & Surgical Incisions Care
- General Anaesthesia: Principles & Risks
- Regional Anaesthesia Types & Uses
- Hypoxia: Causes, Signs & Treatment
- Surgical Infections: Prevention & Management
- Post-Op Surgical Infections: Specific Types
- Sepsis: Recognition & Urgent Treatment
- Systemic Inflammatory Response Syndrome (SIRS)
- Shock: Types & Clinical Management
- Acute Kidney Injury (AKI): Causes & Treatment
- Fractures: Types & Healing
- Congenital Childhood Orthopaedic Disorders
- Metabolic & Infective Bone Disorders
- Arthritis: Types & Management
- Musculoskeletal Tumours Overview
- Burns: Assessment & Treatment
- Major Trauma: Initial Management
- Traumatic Brain Injury: Nursing & Care
- GERD: Gastro-oesophageal Reflux Disease
- Oesophageal Carcinoma: Signs & Treatment
- Peptic Ulcer Disease (PUD)
- Gastric Carcinoma: Diagnosis & Care
- Malabsorption: Symptoms, Causes & Treatment
- Crohn’s Disease: Symptoms & Treatment
- Acute Appendicitis: Symptoms & Treatment
- Diverticular Disease: Symptoms & Treatment
- Ulcerative Colitis: Symptoms & Treatment
- Colorectal Carcinoma: Symptoms & Treatment
- Benign Anal & Perianal Disorders
- Intestinal Obstruction: Causes & Symptoms
- Abdominal Hernias: Types, Symptoms & Surgery
- Gallstone Disease: Causes & Symptoms
- Gallstone Disease: Diagnosis & Surgery
- Pancreatitis: Causes & Management
- Pancreatic Tumours: Types & Treatment
- Benign Breast Disease
- Breast Cancer: Diagnosis & Treatment
- Goitre: Causes, Symptoms & Treatment
- Thyroid Malignancies: Types & Symptoms
- Parathyroid Disease: Symptoms & Causes