What is Myasthenia Gravis?
Myasthenia Gravis (MG) is a chronic autoimmune neuromuscular disorder that causes weakness and rapid fatigue of voluntary muscles. It’s most commonly due to autoantibodies targeting acetylcholine receptors (AChR) at the neuromuscular junction, impairing signal transmission.
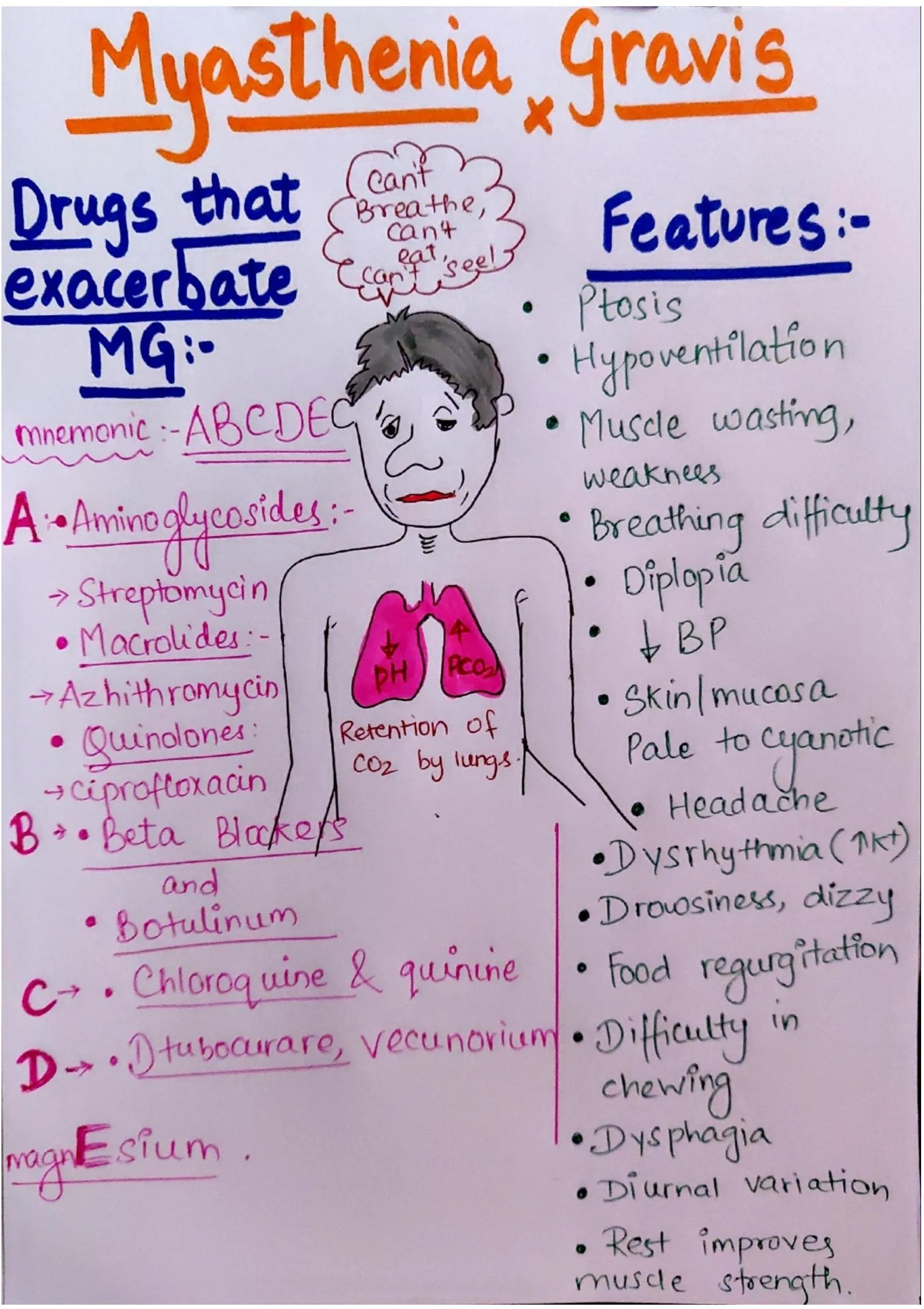
MG literally means “grave muscle weakness,” and it manifests most commonly with symptoms like ptosis, diplopia, difficulty in chewing, dysphagia, and generalized fatigue.
Understanding the Pathophysiology
MG is an autoimmune disease where:
- Antibodies bind to ACh receptors on the post-synaptic membrane.
- This blocks or destroys these receptors.
- The result? Decreased neuromuscular transmission and muscle fatigue.
Sometimes, antibodies may also target MuSK (Muscle-Specific Kinase) or LRP4.
Common Symptoms of Myasthenia Gravis
According to the visual and medical literature, here are hallmark features:
- Ptosis – drooping eyelids
- Diplopia – double vision
- Hypoventilation – shallow breathing
- Muscle weakness (increasing with use, improving with rest)
- Fatigability
- Food regurgitation
- Difficulty chewing and swallowing (dysphagia)
- Headache & drowsiness
- Skin/mucosa changes – pale or cyanotic
- Dysrhythmia
- Diurnal variation – worse in the evening
- Respiratory crisis – in severe cases
ABCDE Mnemonic: Drugs That Exacerbate Myasthenia Gravis
A – Aminoglycosides, Macrolides & Quinolones
- Streptomycin, Azithromycin, Ciprofloxacin
- Block neuromuscular transmission
B – Beta Blockers & Botulinum Toxin
- Reduce strength of muscle contraction
C – Chloroquine & Quinine
- Used in malaria; affect synaptic transmission
D – D-Tubocurarine & Vecuronium
- Neuromuscular blocking agents used in surgery
E – Magnesium
- Inhibits calcium channels → impairs neurotransmitter release
Pro Tip for Students: "Avoid ABCDE drugs in MG" is a fast recall tool for exams and clinical rotations.
How These Drugs Affect Neuromuscular Transmission
| Drug Class | Effect on MG |
|---|---|
| Aminoglycosides | Inhibit ACh release at nerve endings |
| Beta-blockers | Reduce muscle strength |
| Chloroquine | Alters ACh receptor function |
| Curare-type drugs | Compete with ACh at receptor site |
| Magnesium | Reduces ACh release (via calcium block) |
Diagnosis of Myasthenia Gravis
Bedside Tests
- Ice pack test (improves ptosis temporarily)
- Fatigability tests
Lab Tests
- Serum AChR antibodies
- Anti-MuSK antibodies (if AChR negative)
Electrophysiological Studies
- Repetitive Nerve Stimulation (RNS)
- Single-fiber EMG (most sensitive)
Imaging
- CT/MRI chest – to check for thymoma
Differential Diagnosis: What Else Could It Be?
| Condition | How It Differs |
|---|---|
| Lambert-Eaton Syndrome | Improves with use; reflexes reduced |
| Botulism | Pupillary involvement, GI prodrome |
| Motor neuron disease | Spasticity, no improvement with rest |
Treatment Options: Medical & Surgical
First-line
- Pyridostigmine (AChE inhibitor)
Immunosuppression
- Steroids (Prednisolone)
- Azathioprine, Mycophenolate
Crisis Management
- IVIG or Plasma Exchange
- Hospitalization + ventilatory support
Surgery
- Thymectomy: Even without thymoma, it can improve outcomes
Myasthenic Crisis vs. Cholinergic Crisis
| Feature | Myasthenic Crisis | Cholinergic Crisis |
|---|---|---|
| Cause | Under-treatment | Over-treatment |
| Pupils | Normal/dilated | Constricted |
| Secretions | Normal | Excessive salivation |
| Response to Edrophonium | Improves | Worsens |
Lifestyle Modifications & Patient Education
- Avoid overexertion
- Wear eye patches for diplopia
- Eat small, frequent meals
- Schedule rest periods
- Avoid ABCDE drugs
- Inform healthcare providers about MG
Myasthenia Gravis in Special Populations
Pregnancy
- Can worsen in 1st trimester
- Neonatal MG possible (transient)
Children (Juvenile MG)
- More responsive to therapy
- Monitor developmental milestones
Case Study: A Classic Presentation
A 28-year-old woman reports drooping eyelids, difficulty swallowing, and evening fatigue. She started ciprofloxacin 4 days ago for a UTI. Ice pack test was positive. Anti-AChR antibodies confirmed the diagnosis.
Lesson: Always check for contraindicated medications in MG patients.
Mnemonic Recap: ABCDE
| Letter | Drug Class | Examples |
|---|---|---|
| A | Aminoglycosides, Macrolides | Streptomycin, Azithro |
| B | Beta-blockers, Botulinum | Propranolol, Botox |
| C | Chloroquine, Quinine | Malaria meds |
| D | D-Tubocurarine, Vecuronium | Paralytics |
| E | Magnesium | IV MgSO4, Antacids |
Summary Table: Features, Triggers & Management
| Symptom | Explanation | Management |
|---|---|---|
| Ptosis, Diplopia | Ocular muscle fatigue | Pyridostigmine, rest |
| Breathing Difficulty | Diaphragm involvement | ICU + IVIG |
| Dysphagia, Weakness | Bulbar muscle dysfunction | Small meals, AChE inhibitors |
| Drug-induced flare | ABCDE drugs | Stop offending drug |
Final Thoughts and Key Takeaways
- MG is treatable and manageable.
- Symptoms may fluctuate and worsen with fatigue.
- Knowing the ABCDE mnemonic helps avoid medication pitfalls.
- Prompt treatment can lead to a normal life expectancy.
FAQs on Myasthenia Gravis
Q1. Is Myasthenia Gravis curable?
No, but it’s manageable with lifelong treatment.
Q2. Can you exercise with MG?
Yes, under guidance. Avoid fatigue.
Q3. Are MG patients more prone to infections?
Not inherently, but immunosuppressants may increase risk.
- Atherosclerosis & Risk Factors
- Peptic Ulcer: Key Symptoms
- Trigeminal Neuralgia: Nursing Care
- Drug-Induced Gout: Causes & Management
- ECG Changes in Electrolyte Imbalance
- Hypernatremia: Causes, Signs & Treatment
- Status Epilepticus: Complications & Care
- Mumps: Features & Management
- Arsenic Poisoning: Exposure & Treatment
- Hypoxia: Causes, Detection & Treatment
- Mercury Poisoning: Symptoms & Management
- Myasthenia Gravis: Pathophysiology & Nursing Care
- Jaundice & Cholestasis: Overview & Causes
- Hepatitis: Treatment Options
- Exercise Strategies for Diabetics
- Alcoholic Liver Disease: Causes & Care
- Heat Stroke: Symptoms & First Aid
- Abdominal Pain: Diagnoses & Evaluation
- Macrocytic Anaemia: Causes & Treatment
- Hypersensitivity Reactions Types & Management
- Hyperkalemia: Causes & Management
- Drugs Causing Porphyria: What to Know
- Haemoptysis: Causes & Urgency
- Enuresis: Types & Management
- Asthma: Causes, Symptoms & Treatment
- Pleural Disease: Types & Clinical Features
- Pulmonary Embolism (PE): Diagnosis & Care
- Splenomegaly: Causes & Examination
- Hepatic Encephalopathy: Signs & Management
- Reversible Dementia: Common Types
- Emphysema: Signs & Symptoms
- Malignant Pleural Effusion: Clinical Notes
- Sepsis: Recognising Clinical Signs
- Lung Cancer: Early Symptoms to Watch
- Fever With Rash: Differential Diagnoses
- Parkinsonism Features & Causes
- Cerebral Palsy: Types & Management
- Organisms Causing Bloody Diarrhea
- Tremors: Types & Causes
- Psychiatric Patient Assessment
- Knee Pain: Common Causes & Care
- Pediatric Fever: Assessment & Treatment
- Renal Failure After Cardiac Surgery
- Neurovascular Assessment: How to Check
- Carpal Bones: Anatomy & Injuries
- Crohn’s Disease: Overview & Care
- Hypovolaemic Shock: Causes & Emergency Management
- Jaundice: Types, Causes & Management
- Hypercalcemia: Causes & Symptoms
- Muscular Dystrophy: Types & Care
- Cholera: Prevention & Management
- Severe Dehydration: Signs & Treatment
- Influenza: Symptoms & Nursing Care
- Acute Respiratory Illness: Protocols & Care
- CREST Syndrome / Systemic Sclerosis
- Congestive Heart Failure: Management & Signs
- Stable Angina: Presentation & Treatment
- Infective Endocarditis: Causes & Treatment
- Dementia: Types & Care Strategies
- Hashimoto’s Thyroiditis: Symptoms & Treatment
- Functions of Blood: What Blood Does in the Body
- Thyroid Blood Supply Anatomy
- Laryngeal Cartilages: Anatomy & Function
- Clubbing: Causes and Clinical Significance
- Antibiotic Sensitivity Tests: How They Work
- Stroke: Types, Symptoms & Acute Care
- Hypocalcemia: Low Calcium Causes & Treatment
- Apgar Score: Assessment of Newborn Health
- TORCH Infections in Pregnancy: Overview
- Substances That Cross the Placenta: What to Know
- Chronic Cough: Causes & Investigations
- Macrocytosis: Enlarged Red Cells Causes
- Hypoxaemia: Causes & Management
- Horner’s Syndrome: Features & Causes
- Kawasaki Disease: Presentation & Treatment
- Asthma: Treatment Options & Guidelines
- Pancreatitis: Causes, Complications & Management
- Pulmonary Fibrosis: Causes & Learn-TEA
- Chronic Bronchitis: Causes & Care
- Cavernous Sinus: Anatomy & Contents
- Aortic Valve Replacement: When & How
- Naked RNA Viruses: Characteristics & Examples
- Depression: Signs, Types & Treatment
- Causes of Diarrhea: Types & Prevention
- Atrophic Rhinitis: Symptoms & Management
- Staphylococcus aureus: Infections & Treatment
- Duke’s Criteria for Infective Endocarditis
- Hyponatremia: Causes & Treatment
- Fever of Unknown Origin (FUO): Evaluation
- Pancreatitis: Causes & Risk Factors
- Hoarseness of Voice: Possible Causes
- Abdominal Trauma: Assessment & Management
- Eosinophilia: Causes & Workup