Orthopaedic disorders aren't always traumatic—they often stem from metabolic imbalances or infections that alter bone structure, density, and integrity. From common conditions like osteoporosis to potentially life-threatening infections like osteomyelitis, understanding these disorders is vital for timely diagnosis and treatment.
What Are Metabolic Bone Diseases?
Metabolic bone diseases result from abnormal bone remodeling—due to hormonal, nutritional, or genetic factors. They may cause bone loss, deformity, fractures, or growth disturbances in children.
Bone Remodeling:
- Osteoblasts build bone
- Osteoclasts break it down
- Imbalance leads to weakened bone
Common Metabolic Bone Disorders
1. Osteoporosis
Definition: Systemic skeletal disorder with low bone mass and micro-architectural deterioration of bone tissue.
Primary Osteoporosis:
- Postmenopausal women
- Elderly (senile osteoporosis)
Secondary Causes:
- Steroids, rheumatoid arthritis, Cushing's, chronic kidney disease, immobilization
Clinical Features:
- Fragility fractures (hip, spine, wrist)
- Progressive kyphosis
- Back pain
Diagnosis:
- DEXA Scan: T-score < -2.5
- Serum calcium/phosphate: Normal
Treatment:
Lifestyle: Calcium, Vitamin D, smoking cessation, exercise
Pharmacological:
- Bisphosphonates (alendronate)
- SERMs (raloxifene)
- hPTH analogs (teriparatide)
- Denosumab
- Fall prevention, hip protectors
2. Osteomalacia / Rickets
Cause: Vitamin D deficiency → poor mineralization
- Osteomalacia = adults
- Rickets = children
Features:
- Bone pain, tenderness
- Proximal muscle weakness
- Bowing of legs (rickets)
- Looser’s zones (pseudo-fractures)
Diagnosis:
- ↓ Serum calcium and phosphate
- ↑ ALP
- X-rays: widening of epiphysis, cupping
Treatment:
- Vitamin D and calcium supplements
3. Osteolysis
- Bone resorption from malignancy, infection, or post-arthroplasty
- Lytic lesions
- Treatment depends on cause: chemo, surgical excision
4. Hyperparathyroidism
- ↑ PTH → ↑ bone resorption → bone cysts
- Brown tumors, bone pain, fractures
5. Dysplasia
a. Paget’s Disease
- Disorganized bone remodeling with increased turnover
- Affects pelvis, femur, skull, spine
- Pain, deformity, deafness, cardiac failure (high output)
X-ray: Sabre tibia, skull thickening
Treatment: Bisphosphonates, pain relief
b. Marble Bone Disease (Osteopetrosis)
- Dense bones, but brittle
- Risk of fractures, anemia
c. Fibrous Dysplasia
- Replacement of bone with fibrous tissue
- Bowing deformities
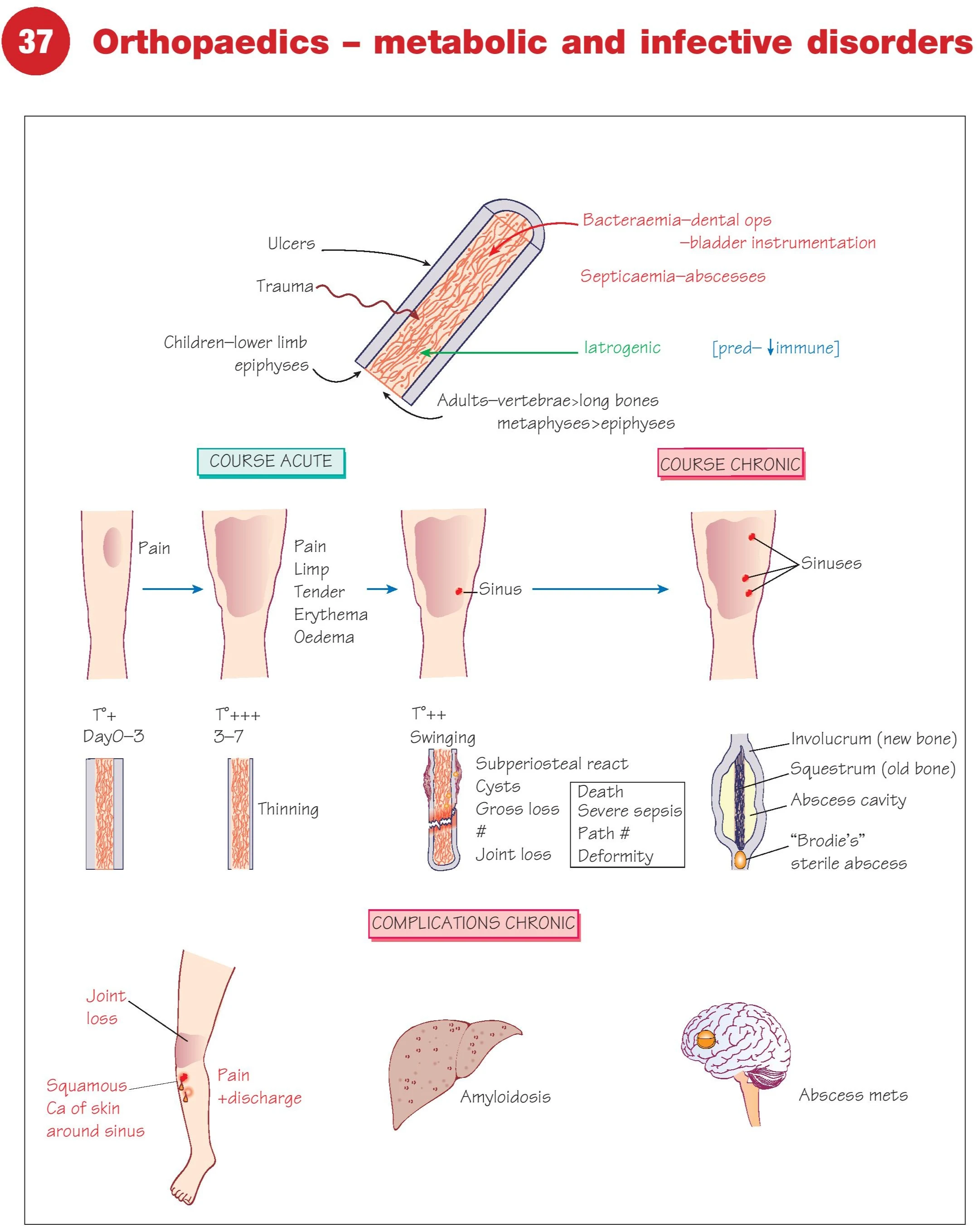
Bone Infections (Osteomyelitis and Others)
Bone infections are urgent orthopaedic concerns. They may be acute or chronic and require antibiotics, drainage, or surgical debridement.
1. Acute Osteomyelitis
- Common in children: tibia, femur
- Organisms: Staphylococcus aureus, Haemophilus influenzae
Symptoms:
- Fever, pain, local tenderness
- Limp or refusal to bear weight
- Swelling, erythema
Phases:
- Day 0–3: Pain, tenderness
- Day 3–7: Erythema, oedema, systemic symptoms
- After 1 week: Sinus formation possible
Diagnosis:
- CBC, ESR, CRP
- Blood cultures
- MRI (best for early detection)
- X-rays (later stages)
Treatment:
- IV antibiotics (6 weeks)
- Surgical drainage if abscess
2. Chronic Osteomyelitis
- Progresses from inadequately treated acute infection
- Sinus formation → persistent discharge
- Sequestrum: dead bone
- Involucrum: new bone formation
- Brodie’s abscess: subacute, well-circumscribed sterile abscess
Complications:
- Joint loss
- Amyloidosis
- Squamous cell carcinoma around sinus
- Brain abscess/metastasis in severe cases
3. Septic Arthritis
- Joint infection via hematogenous spread or trauma
- Red, swollen, painful joint
- Restricted movement
- Common sites: hip, knee
Diagnosis:
- Joint aspiration (purulent fluid)
- MRI/USG
Treatment:
- Joint washout + IV antibiotics
4. Tuberculous Osteomyelitis (Pott’s Disease)
- Hematogenous TB affecting spine
- Common in thoracolumbar region
- Back pain, spinal deformity, fever, weight loss
Diagnosis:
- ESR ↑, X-ray (vertebral collapse)
- MRI spine
- Biopsy for confirmation
Treatment:
- Anti-TB drugs: RIPE regimen (18 months)
- Surgery for abscess drainage or deformity
5. Poliomyelitis (Infective Neuropathy)
Viral anterior horn cell infection
Causes flaccid paralysis and limb deformityManaged via:
- Orthotic support
- Tendon transfers
- Contracture release
Bone Infection Progression (Visual Summary)
- Day 0–3: Local pain
- Day 3–7: Erythema, oedema
- >7 days: Abscess, sinus, systemic sepsis
- Chronic: Bone deformity, draining sinus, sequestrum/involucrum
Chronic Osteomyelitis – Complications
| Complication | Description |
|---|---|
| Joint loss | Due to articular surface damage |
| Sinus carcinoma | Squamous cell carcinoma |
| Amyloidosis | From chronic inflammation |
| Brain abscess/metastasis | From prolonged sepsis spread |
Key Points Recap
- 98% of calcium is stored in bone – critical for skeletal health
- 30% of women will experience osteoporotic fractures
- Acute osteomyelitis needs prompt IV antibiotics
- Chronic osteomyelitis requires surgical debridement
- Bone loss is preventable with lifestyle + pharmacological therapy
Prevention of Metabolic & Infective Bone Disorders
- Calcium & Vitamin D from childhood
- Sunlight exposure
- Weight-bearing exercise
- Early infection control in trauma or post-op cases
- Avoid long-term steroids unless medically essential
- Screening for osteoporosis in postmenopausal women
Frequently Asked Questions (FAQs)
1. Can osteoporosis be reversed?
No, but it can be controlled and fractures can be prevented with lifestyle and medications.
2. How is osteomyelitis diagnosed early?
MRI and blood tests (ESR, CRP) are most sensitive early on.
3. What’s the difference between rickets and osteomalacia?
Rickets affects growing bones in children; osteomalacia is in adults with defective mineralization.
4. Is chronic osteomyelitis curable?
Yes, with complete debridement, long-term antibiotics, and removal of infected tissue.
5. Why does spinal TB cause deformity?
Destruction of vertebral bodies leads to gibbus deformity or collapse.
Conclusion
Metabolic and infective orthopaedic disorders are preventable and manageable—but only with early detection and proper care. Whether it’s correcting calcium deficiency, managing infections, or supporting post-fracture healing, bone health is foundational to whole-body health.
Let’s not take it for granted—strong bones, strong life.
- Neck Lump: Causes, Diagnosis & Treatment
- Dysphagia: Causes, Diagnosis & Treatment
- Haemoptysis: Causes, Diagnosis & Treatment
- Breast Lump: Causes, Diagnosis & Treatment
- Breast Pain: Causes, Diagnosis & Treatment
- Nipple Discharge: Causes & Diagnosis
- Upper GI Bleeding: Causes & Diagnosis
- Lower GI Bleeding: Causes & Diagnosis
- Dyspepsia: Causes, Symptoms & Treatment
- Acute Abdominal Pain: Causes & Diagnosis
- Chronic Abdominal Pain: Causes & Diagnosis
- Abdominal Swelling: Causes & Diagnosis
- Upper Abdominal Swelling: Causes
- Epigastric & Umbilical Abdominal Swelling
- Lower Abdominal Swelling: Causes
- Jaundice: Causes, Types & Diagnosis (LFT)
- Diarrhoea: Causes, Types & Diagnosis
- Altered Bowel Habit & Constipation
- Groin Swelling: Causes & Diagnosis
- Claudication: Leg Pain on Walking
- Acute Warm Painful Leg: Possible Causes
- Acute Cold Leg: Causes & Emergency
- Leg Ulceration: Types & Treatment
- Dysuria: Painful Urination
- Urinary Retention: Causes & Management
- Haematuria: Blood in Urine
- Scrotal Swellings: Differential Diagnosis
- Stomas & Surgical Incisions Care
- General Anaesthesia: Principles & Risks
- Regional Anaesthesia Types & Uses
- Hypoxia: Causes, Signs & Treatment
- Surgical Infections: Prevention & Management
- Post-Op Surgical Infections: Specific Types
- Sepsis: Recognition & Urgent Treatment
- Systemic Inflammatory Response Syndrome (SIRS)
- Shock: Types & Clinical Management
- Acute Kidney Injury (AKI): Causes & Treatment
- Fractures: Types & Healing
- Congenital Childhood Orthopaedic Disorders
- Metabolic & Infective Bone Disorders
- Arthritis: Types & Management
- Musculoskeletal Tumours Overview
- Burns: Assessment & Treatment
- Major Trauma: Initial Management
- Traumatic Brain Injury: Nursing & Care
- GERD: Gastro-oesophageal Reflux Disease
- Oesophageal Carcinoma: Signs & Treatment
- Peptic Ulcer Disease (PUD)
- Gastric Carcinoma: Diagnosis & Care
- Malabsorption: Symptoms, Causes & Treatment
- Crohn’s Disease: Symptoms & Treatment
- Acute Appendicitis: Symptoms & Treatment
- Diverticular Disease: Symptoms & Treatment
- Ulcerative Colitis: Symptoms & Treatment
- Colorectal Carcinoma: Symptoms & Treatment
- Benign Anal & Perianal Disorders
- Intestinal Obstruction: Causes & Symptoms
- Abdominal Hernias: Types, Symptoms & Surgery
- Gallstone Disease: Causes & Symptoms
- Gallstone Disease: Diagnosis & Surgery
- Pancreatitis: Causes & Management
- Pancreatic Tumours: Types & Treatment
- Benign Breast Disease
- Breast Cancer: Diagnosis & Treatment
- Goitre: Causes, Symptoms & Treatment
- Thyroid Malignancies: Types & Symptoms
- Parathyroid Disease: Symptoms & Causes