Introduction: Why Electrolytes Matter in ECGs
Electrolytes like potassium and calcium are essential for cardiac conduction and muscle contraction. Their imbalances can profoundly affect the heart's electrical rhythm, which can be easily detected on an electrocardiogram (ECG).
Even small shifts in serum electrolyte levels can lead to life-threatening arrhythmias, making it critical for medical students, nurses, and doctors to interpret these ECG changes quickly and accurately.
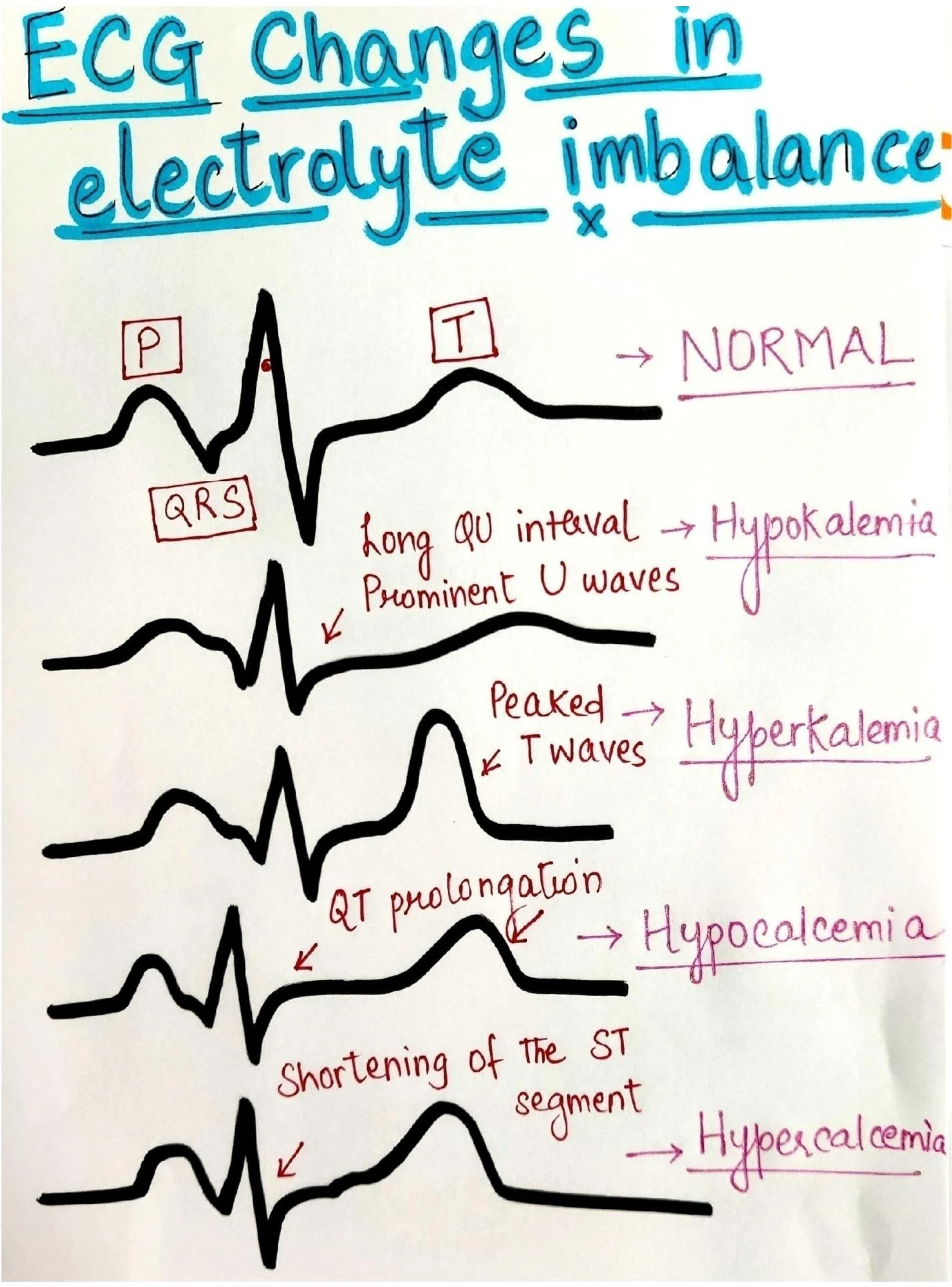
Normal ECG Interpretation: Quick Overview
Before diving into abnormal patterns, let’s quickly revise a normal ECG waveform:
- P wave: Atrial depolarization
- QRS complex: Ventricular depolarization
- T wave: Ventricular repolarization
- U wave: May be visible in certain cases
- PR interval: Atrial impulse conduction time
- QT interval: Total time of depolarization and repolarization
Common Electrolyte Imbalances and ECG Findings
1 Hypokalemia (↓ K⁺)
ECG Findings:
- Prolonged QU interval
- Prominent U waves
- Flattened T waves (not shown in the diagram but often present)
Clinical Impact:
- Increased risk of arrhythmias
- Often seen in diuretic therapy, vomiting, or diarrhea
2 Hyperkalemia (↑ K⁺)
ECG Findings:
- Tall, peaked T waves
- Shortened QT interval (not always)
- Widened QRS in severe cases
Clinical Impact:
- Cardiac arrest risk if K⁺ > 6.5 mmol/L
- Seen in renal failure, potassium-sparing diuretics
3 Hypocalcemia (↓ Ca²⁺)
ECG Findings:
- QT interval prolongation
- Can lead to Torsades de Pointes
Clinical Impact:
- Muscle spasms (Chvostek’s and Trousseau’s signs)
- Seen in vitamin D deficiency, parathyroid dysfunction
4 Hypercalcemia (↑ Ca²⁺)
ECG Findings:
- Shortened ST segment
- May appear as a short QT interval
Clinical Impact:
- Weakness, lethargy, and kidney stones
- Seen in hyperparathyroidism, malignancy
Visual ECG Changes by Electrolyte Type
| Electrolyte | ECG Change |
|---|---|
| Normal | Standard P-QRS-T configuration |
| Hypokalemia | Long QU interval, Prominent U waves |
| Hyperkalemia | Peaked T waves |
| Hypocalcemia | QT prolongation |
| Hypercalcemia | Shortened ST segment |
The image clearly illustrates waveform shifts, making it an excellent revision or flashcard aid for medical students.
Mechanisms Behind ECG Changes
- Potassium affects repolarization, mainly the T wave and U wave. Low K⁺ slows repolarization; high K⁺ speeds it up.
- Calcium primarily impacts the ST segment and QT interval. Low Ca²⁺ prolongs repolarization (long QT), while high Ca²⁺ shortens it.
Understanding the physiology behind ECG changes ensures better recall and helps avoid life-threatening diagnostic errors.
Clinical Relevance of Recognizing These Changes
- Emergency physicians often spot hyperkalemia from ECG even before lab reports arrive.
- Prolonged QT from hypocalcemia can cause Torsades de Pointes, requiring immediate magnesium sulfate.
- ICU monitoring for electrolyte shifts prevents cardiac arrest in septic or renal patients.
Common Conditions That Lead to Electrolyte Imbalance
- Hypokalemia: Vomiting, diarrhea, loop diuretics
- Hyperkalemia: Renal failure, ACE inhibitors, potassium supplements
- Hypocalcemia: Hypoparathyroidism, pancreatitis
- Hypercalcemia: Cancer, vitamin D intoxication, hyperparathyroidism
How to Quickly Spot Electrolyte Disturbances on ECG
| Visual Clue | Likely Cause |
|---|---|
| Tall T wave only | Hyperkalemia |
| Prolonged QT + spasm | Hypocalcemia |
| Flat T + U wave | Hypokalemia |
| Short QT (ST segment ↓) | Hypercalcemia |
Train yourself to mentally match the waveform patterns to electrolyte profiles.
Management and Treatment Principles
- Always confirm with serum electrolyte panel
- Treat underlying cause (e.g., vomiting, renal failure)
- Hypokalemia: Oral or IV potassium chloride
- Hyperkalemia: Calcium gluconate, insulin + glucose, dialysis
- Hypocalcemia: IV calcium gluconate
- Hypercalcemia: IV fluids + bisphosphonates
ECG vs. Blood Test: What Comes First?
- ECG is often the first clue, especially in emergency settings.
- However, always corroborate with serum labs before initiating aggressive therapy.
- In high-risk patients, keep ECG monitoring continuous.
Real-World Case Scenarios
Case 1:
A 67-year-old dialysis patient with missed sessions presents with muscle weakness. ECG shows tall T waves and widened QRS. → Diagnosis: Hyperkalemia
Case 2:
A 34-year-old woman with pancreatitis complains of tingling. ECG shows prolonged QT interval. → Diagnosis: Hypocalcemia
Summary Table: ECG Changes in Electrolyte Imbalance
| Electrolyte | QT Interval | T Wave | U Wave | ST Segment |
|---|---|---|---|---|
| Hypokalemia | ↑ (QU) | Flattened | Prominent | Normal |
| Hyperkalemia | Normal or ↓ | Peaked | Absent | Normal or depressed |
| Hypocalcemia | ↑ | Normal | Normal | Prolonged |
| Hypercalcemia | ↓ | Normal | Normal | Shortened |
Mnemonics & Memory Aids
For Potassium:
- "Low K = Long U" → Hypokalemia = Long QU + U wave
- "High K = Tall T" → Hyperkalemia = Peaked T wave
For Calcium:
- “Low Ca = Long QT”
- “High Ca = Short QT”
FAQs on ECG Changes in Electrolyte Imbalance
Q1: What’s the earliest sign of hyperkalemia on ECG?
A: Tall, peaked T waves are the earliest and most specific sign.
Q2: Can hypocalcemia be confused with long QT syndrome?
A: Yes, both prolong the QT interval but need clinical correlation.
Q3: Which electrolyte disturbance is most dangerous?
A: Hyperkalemia due to its risk of sudden cardiac arrest.
Q4: How quickly can ECG normalize after correction?
A: Within minutes to hours, depending on severity and treatment speed.
Q5: Is U wave always pathological?
A: Not necessarily. It becomes significant when prominent or visible in multiple leads, especially in hypokalemia.
Key Takeaways & Final Words
- ECG is a fast, cost-effective way to detect electrolyte imbalance.
- Hypokalemia → long QU, U wave. Hyperkalemia → peaked T.
- Hypocalcemia → QT prolongation, Hypercalcemia → short ST/QT.
- Rapid recognition = life-saving intervention.
- Keep practicing ECGs to master this essential diagnostic skill.
- Atherosclerosis & Risk Factors
- Peptic Ulcer: Key Symptoms
- Trigeminal Neuralgia: Nursing Care
- Drug-Induced Gout: Causes & Management
- ECG Changes in Electrolyte Imbalance
- Hypernatremia: Causes, Signs & Treatment
- Status Epilepticus: Complications & Care
- Mumps: Features & Management
- Arsenic Poisoning: Exposure & Treatment
- Hypoxia: Causes, Detection & Treatment
- Mercury Poisoning: Symptoms & Management
- Myasthenia Gravis: Pathophysiology & Nursing Care
- Jaundice & Cholestasis: Overview & Causes
- Hepatitis: Treatment Options
- Exercise Strategies for Diabetics
- Alcoholic Liver Disease: Causes & Care
- Heat Stroke: Symptoms & First Aid
- Abdominal Pain: Diagnoses & Evaluation
- Macrocytic Anaemia: Causes & Treatment
- Hypersensitivity Reactions Types & Management
- Hyperkalemia: Causes & Management
- Drugs Causing Porphyria: What to Know
- Haemoptysis: Causes & Urgency
- Enuresis: Types & Management
- Asthma: Causes, Symptoms & Treatment
- Pleural Disease: Types & Clinical Features
- Pulmonary Embolism (PE): Diagnosis & Care
- Splenomegaly: Causes & Examination
- Hepatic Encephalopathy: Signs & Management
- Reversible Dementia: Common Types
- Emphysema: Signs & Symptoms
- Malignant Pleural Effusion: Clinical Notes
- Sepsis: Recognising Clinical Signs
- Lung Cancer: Early Symptoms to Watch
- Fever With Rash: Differential Diagnoses
- Parkinsonism Features & Causes
- Cerebral Palsy: Types & Management
- Organisms Causing Bloody Diarrhea
- Tremors: Types & Causes
- Psychiatric Patient Assessment
- Knee Pain: Common Causes & Care
- Pediatric Fever: Assessment & Treatment
- Renal Failure After Cardiac Surgery
- Neurovascular Assessment: How to Check
- Carpal Bones: Anatomy & Injuries
- Crohn’s Disease: Overview & Care
- Hypovolaemic Shock: Causes & Emergency Management
- Jaundice: Types, Causes & Management
- Hypercalcemia: Causes & Symptoms
- Muscular Dystrophy: Types & Care
- Cholera: Prevention & Management
- Severe Dehydration: Signs & Treatment
- Influenza: Symptoms & Nursing Care
- Acute Respiratory Illness: Protocols & Care
- CREST Syndrome / Systemic Sclerosis
- Congestive Heart Failure: Management & Signs
- Stable Angina: Presentation & Treatment
- Infective Endocarditis: Causes & Treatment
- Dementia: Types & Care Strategies
- Hashimoto’s Thyroiditis: Symptoms & Treatment
- Functions of Blood: What Blood Does in the Body
- Thyroid Blood Supply Anatomy
- Laryngeal Cartilages: Anatomy & Function
- Clubbing: Causes and Clinical Significance
- Antibiotic Sensitivity Tests: How They Work
- Stroke: Types, Symptoms & Acute Care
- Hypocalcemia: Low Calcium Causes & Treatment
- Apgar Score: Assessment of Newborn Health
- TORCH Infections in Pregnancy: Overview
- Substances That Cross the Placenta: What to Know
- Chronic Cough: Causes & Investigations
- Macrocytosis: Enlarged Red Cells Causes
- Hypoxaemia: Causes & Management
- Horner’s Syndrome: Features & Causes
- Kawasaki Disease: Presentation & Treatment
- Asthma: Treatment Options & Guidelines
- Pancreatitis: Causes, Complications & Management
- Pulmonary Fibrosis: Causes & Learn-TEA
- Chronic Bronchitis: Causes & Care
- Cavernous Sinus: Anatomy & Contents
- Aortic Valve Replacement: When & How
- Naked RNA Viruses: Characteristics & Examples
- Depression: Signs, Types & Treatment
- Causes of Diarrhea: Types & Prevention
- Atrophic Rhinitis: Symptoms & Management
- Staphylococcus aureus: Infections & Treatment
- Duke’s Criteria for Infective Endocarditis
- Hyponatremia: Causes & Treatment
- Fever of Unknown Origin (FUO): Evaluation
- Pancreatitis: Causes & Risk Factors
- Hoarseness of Voice: Possible Causes
- Abdominal Trauma: Assessment & Management
- Eosinophilia: Causes & Workup